The Life and Times of a General Surgeon
CONTENTS
PHOTOGRAPHS
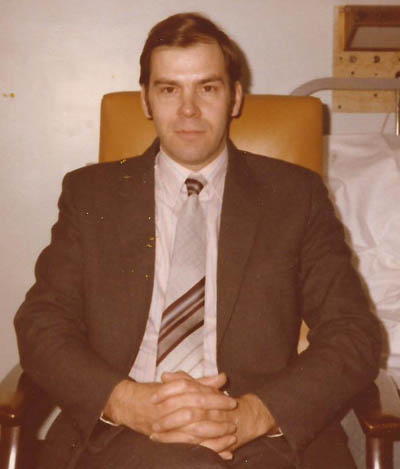
1. 1999 The author photographed by Rayment Kirby.
2. 1963.The Pembroke College Barge on the Isis, re-produced by kind permission of the Master, Fellows and Scholars of Pembroke College, Oxford.
3. 1967. St Thomas’s Hospital Boat Club Four.
Also by the author:
The End of the Golden Age of General Surgery. 1870-2000.
The Training and Practice of a General Surgeon in the Late Twentieth Century. 2014.
ISBN: 1499531370. ISBN 13: 9781499531374. Library of Congress Control Number: 2014908865. (To be found on Amazon as soft back book or Kindle version).
CHAPTER 1: Seven years as a medical student.
In the autumn of 1962 I went up to Pembroke College, Oxford to read medicine. The academic side of life has already been described*.
Pembroke College, formerly Broadgates Hall was founded in 1624 by letters patent signed by King James and was named after the Earl of Pembroke. It was one of the University’s smaller colleges. A friendly place with beautiful quadrangles covered by ancient ivy and set off by window boxes overflowing with flowers in the summer. The college was affectionately known as “Pemmy”. Tom Tower, the magnificent entrance to Christ Church, looks straight down on Pemmy whose walls were black. Then in the nineteen-sixties the blackness was a relic of the smoke and soot of the industrial revolution of the 18th and 19th centuries, this soot had earned Pemmy the soubriquet of “Christ Church’s coal-scuttle”. By the 21st century all that grime has gone, the ivy removed and the walls restored to a pristine condition, the window boxes in summer are still stunning.
My rooms were on the fourth floor of staircase six of Chapel Quadrangle, sometimes called the second quadrangle, which was next to the Hall and the cellar. It could not have been more conveniently placed as friends would drop in for a chat on their way to hall for dinner. The atmosphere in the quad was succinctly summed up by John Betjeman, in his poem. ‘Summoned by Bells’, that was first broadcast in 1976, fourteen years after I had inhabited the top room on staircase six in second quad:
How empty, creeper-grown and odd
Seems lonely Pembroke’s second quad
Still, when I see it, do I wonder why?
That college so polite and shy
Should have more character than Queen’s
Or Univ, splendid in the High.
So for my first year I was the happy denizen of a large sitting-room cum study looking down on the second quad. There was a bedroom and a scullery at the back with a separate staircase for the scout to use. My scout, George Dawson, was the best there was. George was discreet and didn’t tidy up any papers even if they had been carelessly “filed” all over the floor. He brought a cup of tea in every morning and imparted any news he thought worthy of mention. If a visitor came when he was around, he would just melt away.
Years later in nineteen-sixty-nine, when I was collecting my degrees of Bachelor of Arts, Bachelor of Medicine and Bachelor of Surgery and then also eleven years later in nineteen-eighty when I received a Doctorate of Medicine, it was George who arranged the hire of the gowns and brought them to the Sheldonian Theatre for the degree ceremonies.
I joined the Boat Club and rowed enthusiastically. The Pembroke VIII had not been Head of the River since 1873. Now ninety years later in 1963 the VIII was languishing in the second division. In 2010 I had occasion to write a letter to the then Captain of Boats returning two books that I have had in my possession for many years. The History of the Rules and Regulations of the Pembroke College Boat Club, dated 1907 and the second was the Rules and Regulations of the Pembroke College Boat Club, printed in 1851.
On the final day of Eights Week races in 1964 the Pembroke Barge splendidly, painted in the college colours of cerise and white and moored to the bank of the Isis almost opposite the University Boathouse had a spacious deck which was ideal for watching the Bumps (races), being several feet above the waterline and so giving a clear view down the river. That day the deck of the barge was crowded with spectators.
As the boats of the first First Division, the final race appeared, everyone rushed to the river-side rail to get a better view. Suddenly there was an almighty crack as one of the mooring chains gave way and then a few seconds later the second chain also snapped with a loud crack. There was now nothing to hold the Barge and with the weight of the surprised spectators on deck, the barge started to list into the Isis.
I suddenly realised that as Captain of Boats I was in charge and as by now the Barge was listing at about fifteen degrees. I gave a great roar and ordered everybody on the deck to move without running to the riverside of the deck and start an orderly disembarkation. I must have done something right as all complied and reached the safety of shore. The listing continued and the barge came to rest on the bottom of the river at about 30 degrees. It was a sad sight to see the elegant old boat taking in water, but I was relieved that there were no casualties.
The day after the sinking, I revisited the poor old barge and waded along the upside of the stateroom to the cabins at the stern. A locker in the riverside cabin was dry and on opening it these two books were lying on the top shelf which is how I came to possess them.
We did enquire about repairing the barge, but alas the rather small sounding five thousand pounds needed in those far off days was beyond our means. I do not know what happened to the barge. Perhaps someone restored it lovingly and it is still gracing a stretch of the Thames.

During one of my long vacations I was in need of some money so I rang the pathology laboratory at St Thomas’s Hospital and asked if they had any work I could do. To my surprise the answer was yes and I became one of the laboratory’s porters. Instructed to collect all the specimens of blood and other fluids from every ward and outpatients and then deliver them to the laboratory, being fit I did this daily at the double. Then I distributed syringes and needles to the wards as the next task. This was quite heavy work as all the syringes and plungers were glass and were daily re-sterilised in an autoclave after being washed. The needles were also auto-claved and then hand sharpened. From personal experience I can say that even when sharpened they were blunt and painful for the patients. It was some years before the disposable sharp needles and syringes were introduced. I enjoyed a few weeks doing this and earned a little money. Another benefit was I now knew my way to every part of St Thomas’s Hospital, from the wards and laboratories to the subterranean passages, so I knew my way around before I would return in the different role as a clinical student.
There was interesting work going on in the science labs in Oxford. For example, the talk of the Anatomy and Pathology departments in 1963 was the work of Dr J.L. Gowans and E.J. Knight2, later published in 1964.
The problem that they solved was the conundrum of what happens to small lymphocytes (white cells) in response to an infection. It was known that these leave the bloodstream, by traversing the walls of the capillaries to reach an area of infection and then later collect in the regional lymph nodes (glands). What happened to them next?
In an elegant study in rats, Gowans and Knight showed that the small lymphocytes then pass along the lymphatic vessels which join together to form the thoracic duct which discharges the lymph and lymphocytes from most of the body into the left subclavian vein in the neck and so are recirculated in the blood stream. This is important, as although most lymphocytes have a short lifespan some are long lived and provide the immunological memory of past infections, enabling a rapid response to any repeat infection. This work established that lymphocytes circulated through the lymphatics and back into the bloodstream**.

After being awarded a degree in Animal Physiology and passed the preclinical examinations I went as a student to St Thomas’s Hospital in Lambeth in London on the edge of the Thames looking directly across at the Houses of Parliament.
I had the pleasure during the years of clinical study to live at 19 Middleton Square near the Angel of Islington. Middleton Square is a Regency Square with imposing terraces of houses on the four sides of the square, with most houses having five floors. Number 19 has a small patio and garden at the back and at the top of the house the roof was flat, easily accessible and ideal for sitting out on. The house had five spacious bedrooms, a magnificent sitting room on the first floor, a large dining room on the ground floor at the front with the kitchen at the back. There were also two bathrooms and three lavatories. I still marvel that a bunch of students managed to find such a fantastic residence in an elegant house now worth a fortune. Perhaps not, for when I walked in Middleton Square in 2014 I saw that number 19 had been converted into flats and the house looked down at heel.
Residence in this Regency terraced house was made possible by my friend, Paul Clarke, also a medical student, who had been at Oxford. While there he had joined the Royal Navy. On coming down from Oxford he was a Surgeon-Sub-Lieutenant and with the Royal Navy behind him was an ideal tenant for the New River Company who owned Middleton Square and thus obtained a lease on the house.
Paul invited four fellow students to join him. Andrew Pengelly and Andrew Hillyard who had been at Keble College, Mike Mole and I were from Pembroke College. The two Andrews and Mike were clinical students at the Middlesex Hospital, I was at St Thomas’s Hospital known as Tommy’s and Paul was at Bart’s, St Bartholomew’s Hospital.
We arranged to pay £5 2s 6d a week (£5.12 ½p) into a special account in Paul’s name. This covered: the rent, basic foodstuffs, local phone calls and utility bills. There was still enough money left over for one or two parties to be held at the house every year. I do not remember any arguments at all arising from this arrangement, it was very harmonious. We were a fortunate generation as parents paid tuition fees and students whose parents could not afford these fees were given financial help after submitting to a means test and so received a grant from their local County Council, who were generally most supportive. The present system of loans, in the twenty-first century is daunting for modern students, for whatever degree they get they are guaranteed to be in debt when they graduate. A small counter balance in the nineteen-sixties was the low salary of a house officer. After tax and paying for housing the net income was fifteen pounds a month and only a year or before house officers were not paid.
St Thomas’s arranged an introductory course for all new clinical students which lasted six weeks. Oliver Stansfield had been a year ahead of me at Pembroke and had gone to Tommy’s the year before. He told me that there was no need to attend all the introductory course as everything would be covered later. Sadly, Oliver who was an experienced and keen mountaineer, died tragically from a fall in the Alps a year later, a very sad loss.
Having presented myself to the Dean of the Medical School, Mr. R.W. Nevin, I then spent much of the next six weeks on the Thames rowing. I came to know the members of the Hospital Boat Club well and after rowing in various races formed a coxless IV with Rod Thomas, John Black and Richard Collins. The next year this same crew rowed in the ‘Wyfold Fours’ event at Henley Royal Regatta and we did reasonably well. Not having had time to train as much as we would have liked we were satisfied with the result. Years later John Black became well known as the President of the Royal College of Surgeons of England.
These few weeks of the introductory course at St Thomas’s was an idyllic interlude between undergraduate and clinical studies. Looking back, it was the longest break from intensive study or work I had until my retirement.
The clinical year was very different from university terms and was continuous with no formal vacations. Each student could take two weeks holiday a year. My parents being abroad during my student days I lived at 19 Middleton Square throughout this time, except when on ‘take’ and living in the hospital one week in four.

I have written about the excitement and broad experience gained as a student while living in the hospital in ‘The End of the Golden Age of General Surgery***’
It was not all hard work and one night when the emergency work had settled down and no-one else was around, three of us played a game in the nineteenth century part of the hospital. We rolled golf balls along the wide and very long corridor on the ground floor of the hospital and the one who rolled it farthest without touching either wall won. This game brought to mind the brilliant architecture of this older part of the hospital.
St. Thomas’s Hospital, thought to have been founded in eleven-seventy-three when Thomas a Becket was canonised, was finally settled on its present site on the bank of the Thames opposite the Houses of Parliament with completion of a new building in eighteen-seventy-one. It consisted of six blocks on three floors, housing out-patient clinics, wards, operating theatres and everything else needed for a hospital, all connected by a single very wide corridor on the ground floor, running the whole length of the building.
This thoroughfare carried all the pedestrian and trolley traffic of the hospital as it was necessary to use this corridor when walking from any part of the hospital to any other. This was a very useful and natural place for casual clinical meetings. For example, two surgical firms with their students while going about their business from one hospital block to another, would cross paths on the ground floor corridor, then stop and talk about patients and topical subjects of mutual interest concerning surgery. The point being that the corridor was wide enough for such a meeting with up to twenty people to take place without obstructing the flow of other people going about their business. It worked brilliantly. It does not translate into modern buildings which are vertical and all movement within the building is by lifts and staircases which do not lend themselves to useful patient orientated casual discussions.
Student days at St Thomas’s while living in Middleton Square were good. Although very busy there was time to study other things and among my interests was the ever growing population of the world.
References.
*The End of the Golden Age of General Surgery. 1870-2000. The Training and Practice of a General Surgeon in the Late Twentieth Century. ISBN 1499531370. Published in 2015 by Amazon. The academic side of life in Oxford is described in this volume.
**J.L. Gowans and E.J. Knight. Proceedings of the Royal Society of London, Series B, Biological Sciences, Vol 159, No 975, (Jan 14, 1964). Pp 257-282.
***Thomas Fairchild (1667-1729). In 1717 Fairchild took pollen from a carnation and inserted it into a Sweet William resulting in successfully fertilisation. The resulting plant was the first recognised man engineered hybrid plant and became known as ‘Fairchild’s Mule’. This caused great interest and a paper was presented to the Royal Society in 1724. Philosophical Transactions (XXXIII. 127). It also caused problems with the Church due to the belief in creation and therefore the immutability of species at that time. Fairchild kept a vineyard and plant nursery in Hoxton, London where the school was named after him.
CHAPTER 2: A houseman’s life.
The lease at 19 Middleton Square finished when student days finally ended. Having been undergraduates at Oxford we returned there for our final examinations in medicine and surgery. Successful in these examinations, the letters BM, BCh, (Bachelor of Medicine and Bachelor of Surgery) could be added to the BA in Animal Physiology already awarded. Now a graduate could be called by the honorary title of Doctor.
At the ceremony in the Sheldonian Theatre in Oxford, those being awarded degrees in Medicine swore the Oath attributed to Hippocrates (460-377 BC) philosopher and physician. This oath lays down the moral code of conduct for doctors. The oath was read in Latin with a cadence and great solemnity. In an august place, surrounded by one’s fellows and a great congregation it was impelling and we all answered “Volo” in loud voices meaning, “I will*”.
My first day at regular work was at the age of 24 when my friend Patrick Wheeler and I were appointed as house surgeons to Mr R.W. Nevin and Mr H.E. Lockhart-Mummery. Mr Nevin was known to the students and junior doctors as “Uncle Bob” and as he was Dean of the Medical School of St. Thomas’s Hospital, this was a prestigious job and I was lucky to have it.
During the week Mr Nevin lived in a flat in Lambeth Palace, just a short walk from the Hospital, and at weekends went home to the country. It was his habit to come into the hospital every weekday at eight o’clock, to be met at the front entrance by the house surgeon who had been on duty the night before and then together, conduct a round of all his patients.
I lived in the hospital for over three months out of my six months as house surgeon. This was because Mr Nevin’s Firm was on ‘Take’ one week in four when both house officers had to live in to look after the emergencies, so I lived in the hospital for fifteen of the twenty-five weeks that I served as a house surgeon. The work done is detailed in my book**.
A pleasant feature of “living in” was eating in the Junior Doctor’s Mess, which was quite luxurious at that time. We sat at long tables, elegantly laid, with stewards serving at meal times. The chef was excellent and his special delight was to produce a fine dinner for special occasions. The resident junior doctors held one mess dinner while I was “on the House”. It was a splendid affair which matched anything a good hotel could produce. All hospital doctors who were not consultants were called “junior doctors” even if forty years of age and about to be appointed as a Consultant.
Also while on the house I had my first introduction to private practice. Mr. Nevin’s private patients were admitted to the tenth floor of the new hospital block and it was my duty to clerk and admit them and then write up progress notes during their stay. I never had the impression that Mr. Nevin had a large private practice but the patients who came under his care were usually well known.
One morning my bleep gave out the emergency call requiring immediate attendance. The message on my bleep simply read, “Ward 10”. My heart bounded as the only patient Mr Nevin had on Ward 10 that week was Mr Harold Macmillan, the former Prime Minister. I ran down the corridor of the old hospital blocks to the lift and quickly reached Ward 10 on the tenth floor of the new casualty building. On the way I had been turning over in my mind the most likely emergencies that might have befallen Mr Macmillan since his operation a few days before. Heart attack, pulmonary embolus secondary to a deep vein thrombosis or reactive haemorrhage following the operation were the most likely candidates. If he had suffered a cardiac arrest, then the medical “cardiac arrest team” would have also been summoned.
During Mr Macmillan’s operation, a few days before, I had been second assistant, holding a retractor for Mr Nevin at the cholecystectomy he had carried out. The first assistant was Mr H.B. Devlin an able and experienced Senior Registrar. The operation was difficult due to dense chronic inflammation that often occurs in an inflamed gallbladder. The operation had been completed without any problem.
On entering Ward 10 I went straight to Mr Macmillan’s room which had a splendid view across the Thames to the Houses of Parliament on the opposite bank. Just as I was a few paces away the senior consultant physician stepped out of Mr Macmillan’s room holding a large vase of flowers which he handed to me saying, “Ah. There you are Maybury, take these flowers away, Mr Macmillan has too many in his room”. To my breathless enquiry about Mr Macmillan’s wellbeing, he gave me a quizzical look, expressing the sentiment of “silly boy” while he said, “Fine”. I replied, “Yes sir”, and did as I was told with a smile not being sure which emotion was uppermost in my mind, relief that no disaster had befallen Mr Macmillan or chagrin at being summoned by emergency bleep to sort out the flowers!
Mr Macmillan was a good patient and no word of distress or complaint crossed his lips despite his discomfort. He did tell me, a few days after the “flowers” incident while I was carrying out my routine late evening visit of all the firm’s patients, that he had a sharp pain in his lower abdomen. His observations were all stable and he looked well. I carried out a careful abdominal examination and as with any other patient a PR examination. There was nothing the matter that minor treatment would not solve which I duly administered.
The next morning at eight I met Mr Nevin at the main entrance and as we walked through the hospital to the wards I told him what I had found and done for his patient on Ward 10. Mr Nevin’s pace slowed down and he gave me a hard look but said nothing. He may have thought that I had gone beyond my remit, but on finding Mr Macmillan cheerful and his pain gone, probably reflected I had only done what housemen were taught to, and ought to do. The matter was not mentioned again.
On another occasion when I visited Mr Macmillan he was very genial and asked me about my career and as that topic of conversation lapsed I ventured to ask whether he regretted no longer being in the House of Commons over the river. “No”, he said, “I’m too old for playing games” and laughed. A few weeks later he was seen on television getting into a taxi, possibly his first outing since his operation and a reporter asked. “How are you Sir”, and after a pause while he thought about it he replied, “Considering the alternative, very well!”
Another of Mr Nevin’s private patients was an Iraqi Air Force General who arrived bringing his own physician with him. I assisted Mr Nevin at the operation on the General and noted that the general’s personal physician insisted on changing and joining us in the operating theatre. He wanted to inspect every stage of the operation and doubtless reported back to the General when he had recovered from the anaesthetic. We were never told the reason for the Iraqi physician’s detailed interest. The Iraqi General gave me a bag of pistachio nuts when he departed for home. A rare treat at that time.
The people of Lambeth in the nineteen-sixties tended to delay seeking help from the hospital for serious surgical problems, such as obstruction of the bowel or acute appendicitis, so it was not uncommon for them to appear in casualty several days after the onset of their condition.
Thus those with obstruction had not infrequently perforated their colon by the time they attended hospital and had severe peritonitis. Due to the seriousness of their condition they were taken swiftly to the operating theatre after rapid intra-venous rehydration whatever the time of day or night. The most popular time for the sufferer to finally give in and come to hospital for help was often late on Friday afternoon. Fortunately, a full service was given at any time of any day of the week, including public holidays.
Assisting at these operations the surgeons always wore a plastic apron under the sterile surgical gown. On opening the abdomen, the foulest stench would fill the theatre and brown liquid would usually pour out. Surgery was kept to a minimum as the mortality of these patients was high so the perforated bowel was resected and the ends brought out as one or two colostomies. The abdomen was carefully washed out with an antiseptic and antibiotics started. If the patient survived and the perforation had been caused by an obstructing cancer of the colon this would be resected a few weeks later, when the patient was fit enough to withstand a more major procedure.
In cases when the appendix was excised it was frequently gangrenous and therefore septic which meant that development of a post-operative pelvic abscess was common. Mr Nevin managed these patients on the ward. The patient would develop a fever and lower abdominal pain. Any such patient was examined by Mr Nevin on his ward-round and the examination included a rectal examination. At first he would often say, “It’s not ripe”. Over a few days the abscess, a collection of pus, would begin to “point”, developing a softness of the rectum where if left alone it might spontaneously rupture. It was safer to drain the abscess surgically.
Then at his next examination Mr Nevin would announce, “Its ripe, sister the scalpel”. The Ward Sister would quickly come back with one. The blade of the scalpel was laid along his index finger so the tip did not protrude. He would pass his index finger with the blade protected into the rectum. He could then feel the abscess bulging down into and compressing the rectum. With the tip of finger on the softest part of the bulge he would slide the scalpel forward into the abscess and then withdraw both blade and finger. Sister had a large kidney dish ready and placed it against the patient and the pus would pour out. This could be up to three quarters of a litre of pus. The patient immediately felt better and as the fever subsided very quickly they were usually ready to be discharged next day and now draining freely the abscess cavity would heal spontaneously. This was a technique I used on such a case as a consultant myself, this complication having become very rare due to early presentation of patients with appendicitis and prophylactic use of antibiotics during the operation when the appendix was removed.
Another process I learned and saw how to manage was the infection and breakdown of the perineal wound following excision of the rectum for severe ulcerative colitis or cancer. In these circumstances the sutures were removed and the wound opened and then washed with antiseptic and packed with gauze, damp with antiseptic and liquid paraffin. These packs were changed daily at first and care was taken to ensure that no pockets of pus remained. Eventually the wound would heal perfectly without any further surgical intervention. Very occasionally, years later, I used this slow, old fashioned but safe technique to heal infected perineal wounds.
All Mr Nevin’s house surgeons were instructed at the beginning of their tenure, that if a Lady from the Palace rang concerning any member of the Queen’s Household with a surgical problem the answer to any request made was to be automatically answered with a, “Yes Madam”. The patient must be admitted immediately and Mr Nevin informed. He was Surgeon to the Queen’s Household and also to the Metropolitan Police, so any
request from this latter quarter was to be responded to similarly.
To progress my career as a budding surgeon the first professional examination had to be negotiated. This was the Primary examination for the Fellowship of the Royal College of Surgeons (FRCS) which could only be sat following the statutory completion of two house officer posts of six months each, one attached to a surgical firm and the other to a medical firm, then post a casualty officer post (Accident & Emergency Senior House Officer) for six months.
Mr Nevin advised me to apply for a casualty officer’s post at St Thomas’s which would last for six months to be followed automatically, if my application was successful, by six months as a Prosector in the Department of Anatomy of the Medical School. I applied, this was a written application without interview as Prosectors were all appointed from within the Hospital. I was very glad to have been successful, not only because it was a good post but, also I had secured employment for a further year provided I could find a house physician’s post first. There was never any security of tenure, or pre-arranged progression of appointments to jobs throughout my training.
I mentioned my immediate problem to Brendan Devlin, the senior registrar, who was very helpful and thought that Dr Peter Reed, a Consultant General Physician with a special interest in gastroenterology who worked in Slough was looking for a house officer and he would give Dr Reed a ring. With this recommendation Dr Reed asked me to attend for an interview at Wexham Park Hospital.
The interview was an informal affair. I arrived on time exactly as instructed and found that Dr Reed was about to start a routine ward round of all his patients and I was to join it.
The doctors on the round were Dr Reed, Dr Prakash his registrar, the house officer, a couple of students, the Ward Sister and me. We went from bed to bed to see the patients and I was asked one or two straight forward clinical questions. What was particularly interesting was the range of conditions from which the unfortunate patients were suffering.
There was a patient, just admitted, with severe untreated thyrotoxicosis with cardiac complications. Several others had ulcerative colitis, one a sprightly ninety-year old lady was having a first attack of this disease. Her diagnosis was confirmed during the round because fibre optic endoscopes were just becoming available and Dr Reed had one which was used in a side ward set aside for the purpose. The lady was duly scoped under sedation to about 30 centimetres from the anus and all on the round got to look down the scope at a typical florid inflammation of the inflamed rectum and sigmoid colon.
Two patients were recovering from heart attacks and one stroke patient was also reviewed. Then there were patients with severe problems caused by diabetes, two being treated for very high blood sugars, hyperglycaemia. Also a patient recovering from a severe episode of extremely low blood sugar or hypoglycaemia. I was very interested.
After the round we had tea in the Ward Sister’s office and when everyone else had dispersed to their routine duties Dr Reed interviewed me. He asked what my career hopes were and what I had been doing at St Thomas’s. This lasted about ten minutes and then he said he had to go and as he was leaving told me I had been appointed. Just like that. This was 1969 and this was how house officers were appointed until the early 1990’s when interviews began to be more formal and arranged centrally.
Wexham Park Hospital on the outskirts of Slough was fairly new, having been opened in 1965 when its design won the architects a prize. The hospital consisted of a central tower seven stories high, with single story arms radiating out like spokes of a wheel from the base of the tower. The doctor’s mess was on the sixth floor of the tower block and the doctor’s residence on the seventh, a splendid place with huge plate glass windows and panoramic views. At the planning stage the hospital consultants saw the plans and were asked for their views. Most were silent but one ENT surgeon asked where the helicopter-pad was to be situated. There was silence among the architects and then one said, “We hadn’t thought of that!”. Wexham Park Hospital was, I believe, the first hospital with an integral helipad!
When I joined the hospital junior staff and was on duty, my room was on the seventh floor When bleeped for an emergency during the night I rushed to the lift and while it descended seven floors put on my trousers and long white coat over my pyjamas and ran to the site of the emergency in my bare feet. It rarely took more than a minute to run and so emergencies were always attended to very quickly. There was one patient who was very grumpy, who noticed that my pyjama top was showing and said “What are you doing sleeping on duty? Aren’t you the night doctor.” To which I replied “Yes and the day doctor too”.
The mess was very lively and there were frequent communal dinners with each course produced by a different person. In view of the international composition of the mess we had splendid food of all types from Europe and Asia. My wife, who was a teacher at a local primary school, organised this and when the time came to leave our friends at Wexham Park and move on, it was proposed at a mess meeting that someone should be found to fill her unofficial post as mess co-ordinator!
When not on duty, the two weekly rota allowed two nights off the first week and three the second, for this we had been allocated a semi-detached house in the village of Ivor Heath not far from the hospital. When we first went to the house the front garden looked neat and the grass was recently mowed and it looked promising.
On opening the front door, a waft of freezing damp air greeted us. The carpets were filthy and on entering another smell, this time of stale cooking became apparent, there was no central heating and we hastened to light a fire in the sitting room. There was some damp coal but nothing that would light it, so we next turned our attention to getting some hot water which was heated by a solid fuel boiler to be lit by a gas poker. Sara struck a match to light the poker and there was a small explosion. Fortunately, Sara was not hurt but there was now no way of heating any water.
The back garden was a shambles, no-one had tried to do anything with it for years. We later discovered that our neighbour, a kind man who suffered from shell shock following the war, was in the habit of keeping our front garden in order, without recompense, because it was a doctor’s house.
The next day my wife rang the hospital secretary’s office to see if a new boiler could be installed, only to be told, “No, because the next tenant might not want hot water”. The logic of this eluded us. Having bought some dry coal and using old newspaper we lit the sitting room fire. Whenever we were in the house, when I was not on duty, the only heating we had was this fire. We had by now removed the decomposing food from the cooker. Every weekend when not on duty we escaped and went to stay with Sara’s parents in the beautiful village of Brightling in Sussex. There we were warm and always made most welcome.
One evening there was a lecture given in the mess by Professor Sir Ian Coote and afterwards I went to speak to him. We had met fourteen years earlier, in Kampala, where he was the Minister of Health in the Colonial Government of Uganda. I was eleven years old when I told my parents that I wanted to be a surgeon and in view of this ambition my father took me to see Professor Coote to discuss what path I should follow to achieve this. The Professor was very kind and told me about the great Teaching Hospitals in London, mentioning particularly St Thomas’s Hospital opposite the Houses of Parliament. That evening at Wexham Park I was able to thank him for his advice and let him know that I was making progress in my ambition and had been a medical student at St Thomas’s.
Reference.
*If the reader wonders whether the new graduates knew what they were agreeing to when affirming the Hippocratic Oath, he or she will be reassured that all were given a translation before the ceremony.
The original oath reads:-
I swear by Apollo Physician, by Asclepius, by Health, by Panacea and by all the gods and goddesses, making them my witnesses, that I will carry out, according to my ability and judgment, this oath and this indenture. To hold my teacher in this art equal to my own parents; to make him partner in my livelihood; when he is in need of money to share mine with him; to consider his family as my own brothers, and to teach them this art, if they want to learn it, without fee or indenture; to impart precept, oral instruction, and all other instruction to my own sons, the sons of my teacher, and to indentured pupils who have taken the physician’s oath, but to nobody else. I will use treatment to help the sick according to my ability and judgment, but never with a view to injury and wrong-doing. Neither will I administer a poison to anybody when asked to do so, nor will I suggest such a course. Similarly, I will not give to a woman a pessary to cause abortion. But I will keep pure and holy both my life and my art. I will not use the knife, not even, verily, on sufferers from stone, but I will give place to such as are craftsmen therein. Into whatsoever houses I enter, I will enter to help the sick, and I will abstain from all intentional wrong-doing and harm, especially from abusing the bodies of man or woman, bond or free. And whatsoever I shall see or hear in the course of my profession, as well as outside my profession in my intercourse with men, if it be what should not be published abroad, I will never divulge, holding such things to be holy secrets. Now if I carry out this oath, and break it not, may I gain for ever reputation among all men for my life and for my art; but if I transgress it and forswear myself, may the opposite befall me.
(Note by the author. The Hippocratic oath has been rewritten many times but seems to get more complicated. In this translation it appears that the practise of abortion is forbidden but it is now legal in the UK. It is thought that a particular means of procuring abortion has been proscribed by Hippocrates, while abortion itself was carried out in those times. Nowadays a doctor must abide by the ethical and legal demands in such a case).
**The End of the Golden Age of General Surgery. 1870-2000. The Training and Practice of a General Surgeon in the Late Twentieth Century. ISBN 1499531370. Published in 2015 by Amazon. The academic side of life in Oxford is described in this volume.
CHAPTER 3: House hunting and tales from casualty.
Once back at St Thomas’s, working as a casualty officer, Sara and I started to look for a house to buy. We were rather naive as between us we had no capital. Not surprisingly after enquiring at several Building Societies, it became apparent that none would give us a mortgage without a ten percent deposit. This seemed to be the end of our aspiration to own a house. Although salaries were small in 1970, it was an era of prosperity with virtually full employment and property especially houses were appreciating in value fast. It was a desirable time to own your own house.
Since leaving Iver Heath, near Wexham Park Hospital , Sara and I were staying with her parents while I commuted to London to work. On my first weekend on duty in casualty, Sara was with her father having a drink in the Swan Inn at Wood’s Corner in Dallington in Sussex. While standing at the bar she was talking to the landlord about the difficulty of getting a mortgage when a man standing next to her introduced himself as Brian French and told her that he might be able to help with a mortgage provided she did not mind borrowing from a Building Society based in Ireland.
This was good news, as we rather fancied living in a picturesque farm house situated locally. Hook’s Farm was old and built in the classic Sussex style with facing tiles on the upper story. However, it was in a very dilapidated condition and in need of much restoration. This property was mentioned to Brian French and that it was for sale at six thousand pounds. he laughed and gently dashed this dream by saying that no building society would lend to an impecunious pair of young people against such a risky property.
Building Societies, he said, would only lend against new houses which could be easily sold. He knowledgeably added that if one bought the first habitable house on a brand new estate, then by the time the last house was built and ready for sale, the price would have risen, so increasing the value of any houses bought first. Brian French then asked where we wanted to live and Sara thought within a short commute from Waterloo Station, perhaps up to a maximum of an hour’s journey to allow me easy access to St Thomas’s Hospital. A few days later we met Brian at his office in Robertsbridge. He had taken a lot of trouble on our behalf and showed us a map of London and the South East on which he had marked Waterloo Station and three new housing developments he had identified. All these estates had just started to be built and were within forty minutes by train of Waterloo Station.
We visited all three estates, but the one which really caught our eye was in Gillingham in Kent, where for three thousand nine hundred pounds a three bed-room terraced house with a separate garage could be purchased. Brian had more good news in that he had arranged a mortgage in principle for us to buy such a property with an Irish Building Society. We never did find out why he thought we might object to an Irish Building Society.
The Gillingham house was an attractive little house with a kitchen-dining room, we had the floor tiled in black and white. The sitting room was at the front with three minute bedrooms upstairs and a tiny fenced garden at the back. It was perfect and we bought it with the mortgage arranged by Brian French for the price quoted.
The day of the move we arrived at the house and waited for the van to arrive with our furniture. By evening nothing had happened and I was unable to contact the removal firm. Fortunately, the house was carpeted but even so we spent a very uncomfortable night especially for Sara who was pregnant. To my relief the furniture arrived the next day. We had bought the second house to be sold on the estate, exactly as anticipated by Brian French its value rose during the following twelve months as the estate was duly completed and all the houses sold. Because the estate in Gillingham was well placed and a pleasant place to live, our house, as predicted sold very quickly for four thousand nine hundred pounds. Now thanks to Brian French we had a respectable deposit for our next house. We were very grateful to him and met him often at the Swan Inn over the next few years.
Sometime later he offered us a house in the main square in Assisi in Italy for six thousand pounds as a holiday house or to let. This was unfortunately beyond our means and regretfully we were not able to take up his offer. The experience of buying a house combined with the mess I had made of the removals whetted Sara’s interest in houses and thereafter she proceeded to buy and sell our subsequent houses, seventeen in all, arranging everything including all the packing and removals.

We liked living in the Gillingham house and were very happy there. It was to this house that our first child, Nicolas, was brought home to after his birth on the second of December nineteen seventy at the General Lying in Hospital in Lambeth. When Sara went into labour we were staying with friends in London so it only took a few minutes to reach the hospital.
It was early evening but very dark inside the hospital as there was no electricity, this being a time of the three-day week, power cuts and refuse piling up in the streets. Once Sara had been admitted, a rather harassed young doctor came in who I knew vaguely. He said he was rushed off his feet and asked me to put a drip up on my wife as he didn’t have time. I was surprised but did as he asked. Then the midwife came in and happily within a short time Nicolas was born. As was customary Sara stayed in hospital for several days. Then we returned to Gillingham delighted with our first child who was a fine boy.
Working in Casualty (Accident and Emergency Department) was interesting, sometimes amusing, and at times tragic. It was the only training post in those days which was worked in shifts, being the only hospital job which did not provide continuity of care as all the patients were either sent home or admitted under the relevant specialty.
Late one Saturday afternoon, when I was one of the Casualty Officers (CO) on duty, two large rugby forwards from the Tommy’s First XV came into casualty together, one with his two front teeth missing and the other with puncture wounds on the top of his head. Have cleaned the latter’s wound and probed the twin scalp punctures; I was surprised to find the missing teeth embedded deep in the scalp. They were in good condition and after extracting and washing them carefully I gave them back to the “toothless” one to take to his dentist. We all had a good laugh especially the casualties. Those were the last years that the St Thomas’s Hospital rugby XV with an England cap in the side, had fixtures with first class clubs including Rossyln Park and the London Irish.
On another occasion there was a sad tale to tell with an unexpected coincidence. One afternoon the telephone rang to say a casualty with a cardiac arrest was being brought in from Waterloo Station. It was normal practice at that time for a CO to go out the forecourt to meet the ambulance and take immediate charge of resuscitation. On the stretcher was a man of about forty who had had the cardiac arrest. I took him to the resuscitation room and made every effort to revive him but to no avail and in due course declared him dead. It transpired that the lady with him was his secretary and she had been seeing him off from Waterloo Station when he had collapsed on the platform. A tragic situation. she insisted on ringing the man’s wife to tell her what had occurred in spite of my offer to do so.
While serving as a casualty officer I was the junior doctor’s mess secretary and so involved in arranging parties and dinners. The doctors from the previous year had departed from the hospital after a terrific end of job party and had omitted to pay the drinks bill of over one hundred pounds to the wine merchant. The new occupants of the mess were none too pleased, but we honoured the debt and paid the bill.
I organised a formal dinner about half way through the job. We invited my former chief Mr Nevin and his wife as the guests of honour. The chef excelled himself and the Nevins greatly enjoyed the occasion and stayed till late. I received a note of thanks from Mr Nevin, which said how much they had enjoyed the occasion, adding that this was the first time they had been to a mess dinner given by the junior doctors.
Each new batch of casualty officers were given a half day off and treated to go “Round the Corner”. This is an obscure way of saying that we were given a guided tour of the Metropolitan Police’s Black Museum of Crime. This was a great privilege as the museum was not open to the public and only available to police officers and invited guests. This visit had been arranged by Mr Nevin, as Dean of the Medical School, who as previously mentioned was surgeon to the metropolitan police.
I am just old enough to remember when the famous and very distinctive white five-pound note was legal tender. Displayed in the museum alongside a genuine white five-pound note was a forgery, which on a casual glance looked real. The story was that the forger was a racing addict. When he ran out of money for his next bet he secreted himself in a lavatory and there took a pre-prepared sheet of white paper of the right size and about the correct texture from his pocket and then drew in black ink a new note from memory, in a few minutes he had a note which was passable as legal tender in the rush of placing a bet with a bookie at the racecourse. Good at drawing he might be, but not very clever as he only managed to pull the stunt a couple of times before being caught and had won nothing. There were other more sinister exhibits concerning famous murders in London.
After six months in Casualty I moved to the Anatomy Department in the pre-clinical part of the Medical School as a Prosector of anatomy. The pay was meagre, but I was fortunate in that I was asked by Mr Frank Cockett’s secretary if I would like to assist Mr Cockett in his private practice during this time and was offered five pounds a leg. Mr Cockett was a general surgeon at St. Thomas’s, nicknamed “the Ace” by the students. The private practice I assisted him with was exclusively stripping varicose veins, hence my being paid by the leg. He operated several evenings a week, in various private hospitals in central London, between five and seven in the evening also occasionally on Saturday mornings. This fitted in very well with my work as prosector.
As was then the custom, Mr Cockett carried his own splendid gold plated surgical instruments with him, including solid gold needles. After sterilisation these latter were hand threaded by the scrub nurse, as this was before the era of atraumatic needles. His car had a number plate beginning with the letters VV and his sailing boat was called Saphena. Quite a charming feminine sounding name as befits a yacht, but in fact a saphenous varix is a significant dilatation of the highest part of the long saphenous vein just before it joins as a tributary the large femoral vein in the groin and is removed as part of the operation of stripping’ varicose veins. Mr Cockett had a good sense of humour.
Several evenings a week I assisted him at these operations and learned his operating technique which gave excellent results with good cosmetic effect. As Mr Cockett’s confidence in me grew, my assisting became more active and sometimes he asked me to close the wounds. The experience of working for Mr Cockett was of great value in my own private practice years later, but of that I had no inkling at the time. One Saturday morning we finished early and he took me to one of the auction houses in Bond Street to admire a picture he fancied of a nineteenth century oil painting of a splendid man-of-war. I expect he bought it at the subsequent auction as he was reputed to have a fine collection of naval paintings.
My six months as a prosector passed quickly and working again on cadavers and teaching students anatomy, honed my knowledge of the foundation science of surgery that served me well in the future. Since we used Gray’s Anatomy as our textbook one of my co-prosectors, John Black, found an error in Gray’s Anatomy and was proud to point it out to the Professor of Anatomy, Professor Davies, who was also the Editor of the next edition of the book.
CHAPTER 4: Experience in Warwick.
In 1971 I travelled to Warwick, having been invited to attend for an interview by Mr John Marsh, Consultant General Surgeon at Warwick Hospital. After meeting him I accompanied him on a ward-round followed by an informal interview and was appointed on the spot as his Surgical Registrar to be based at Warwick Hospital. There was one proviso, that I must pass the Primary FRCS examination to take up the post. I had already completed the jobs stipulated, by the Royal College of Surgeons of England as essential training and all that remained was to sit the exam. This was to test the knowledge of a candidate in the sciences underpinning surgery, anatomy, physiology and pathology. The examination took place at the Royal College of Surgeons in Lincoln’s Inn Fields only two weeks before Mr Marsh was expecting me to be in post.
Post graduate examinations in medicine and surgery are quite unusual in that the results are announced within hours of the last viva taking place. Following a short time waiting nervously, the list of candidates who has passed was posted on the notice board at the Royal College of Surgeons. I found my name had been included, I had passed and could now proceed to Warwick Hospital.
My wife and I had been offered the house usually allocated to the surgical registrar and after a very cursory look I had accepted it. In those days a single person would live in the house rent free, but being married a commercial rent had to be paid.
Just before my appointment started I went to Warwick to start work. Sara had meanwhile contacted an agent to put our house in Gillingham on the market. The agent said he actually had a waiting list of couples who wanted our house which was good news and confirms the buoyancy of the housing market at that time and the wisdom of Brian French as the house was sold very quickly.
There was only one surgical registrar at Warwick Hospital, who inevitably had great responsibility. Warwick Hospital was the only A & E department in South Warwickshire and all accidents and emergencies not only from the town but also from Leamington Spa and Stratford-upon-Avon, including the surrounding countryside were brought in by ambulance.
Sometime later having packed up the house Sara came up to Warwick from Gillingham. She travelled with the removal men in the furniture lorry, with Nick, our babe in arms and Jack our French bulldog. She told me that this experience was new to the removal men and that they were very kind to her and looked after her well on the journey. The alternative would have been a difficult journey by train with several changes in London with Nick and the bulldog.
On arrival in Warwick she saw the hospital’s semi-detached house allocated to me for what it was; dangerous to live in. Not only was it dirty, but the kitchen was only furnished with a large sink, which was chipped with an unhygienic draining board. There was no work surface and the gas cooker was dilapidated and rusting. That was the best part of the house. In the bathroom everything was chipped or cracked. The immersion heater had no thermostatic control, so the water was boiling all the time. The worst of all defects was a crack in the wall extending from the landing into the bathroom which was big enough to put a hand in. Last but not least our neighbour warned us not to put the baby outside in his pram as all the guttering was loose and at risk of falling. I had indeed been carelessly unobservant at my quick look round.
The following day, in a quiet moment, I told my new chief that we would not live in the hospital house and would move out as soon as we had found somewhere to buy. John Marsh was not best pleased. If I moved out what could he offer the next Registrar to live in, as the house was sure to be snapped up by another department. I quietly stuck to my guns and said the house needed extensive building work as well as refurbishment. After some weeks he did come and look round and agreed it was not habitable. I was now grateful that my wife, with natural flair, was arranging everything to do with our housing.
She quickly found and bought a bright, large and comfortable 1960’s house with four bedrooms, 1 Crossfields Road situated only one hundred and fifty yards from the hospital. We settled in quickly. Sara ran an open house for other junior hospital doctors and it was a most enjoyable place to live.
From the moment I started work the phone rang frequently day and night, especially from casualty and the surgical wards, when often a young female voice on the phone would say, “This is Clare Ward” when asking to speak to me. “Who is this Clare Ward who keeps ringing you,” Sara asked. The wards on which I worked were called Rylands and Clare Wards!
My work rota was awesome. In week one I was on duty all seven days, both day and night except for Wednesday afternoon. In the second week my duty rota was from Monday to Friday, day and night, but with the weekend off. Usually I could get away at six or seven on Friday evening. This two-week rotation was then repeated. This was a baptism of fire, but I enjoyed it enormously as under Mr Marsh’s careful tutelage I made rapid progress. I did not mind the hours as I was accumulating experience at a tremendous pace having arrived at Warwick with very little experience of operating. The work was all absorbing and very busy day and night.
There were many times that I started operating at nine in the morning and was still operating at midnight and often on through the night. The way this worked was by adding all acute surgical emergencies coming into casualty during that day and night to my ongoing operating list. Fortunately, casualty was only a few yards away from the operating theatre so between operations I would go and see the new admissions to casualty and there would be time to get any x-rays or blood tests needed before operating.
Looking back this was a most amazingly efficient way to look after patients, as those with acute appendicitis, strangulating femoral or inguinal hernias, perforated duodenal ulcers, acute bowel obstructions were dealt with within hours of coming into hospital. Initially Mr March was frequently in the hospital at night but as I rapidly became more experienced and his confidence in me increased he allowed me to proceed alone knowing I would ring him concerning any difficulty I may have. Within months these lists would now include patients with blood loss following road traffic accidents whose spleen I removed and carried out colostomies on patients with obstructing tumours of the colon. The full list of operations I learned to carry out in my two years at Warwick Hospital are listed in my book ‘The End of the Golden Age of General Surgery*’.
I loved these long lists as operating through the night was usually very peaceful as the interruptions only came from casualty and the hospital was otherwise quiet. Coming home at dawn on a fresh summer’s morning for breakfast was always pleasurable. I was glad that my wife and I had discussed the irregular home life before getting married and she had accepted it then, but now it was the real thing and all was well between us.
When I was late Sara always stayed up and waited for me and we always had a chat and then breakfasted together with Nick, our baby son. This was about the only time that I saw him regularly as I was rarely home before he went to bed. Then having shaved and bathed I was back to the hospital for the day’s work.
As was normal at that time no concessions were made or expected for sleep lost and no lists were ever cancelled because the surgeon had been up all night. I have frequently been asked if these long hours led to mistakes being made. I was never drowsy while working either on the ward, in casualty or in theatre as the work was so fascinating and all absorbing. I was never bored and remained fully alert when working whatever the hour. Being a surgeon is not the same as driving for hours when the monotony would get to a person resulting in overwhelming tiredness, necessitating a stop for a rest as occurred when travelling down to Sussex on our weekends off duty.
Sometimes if there was no indication of when I was going to return home in the night, Sara would ring the hospital switchboard to ask what was happening. The hospital night switchboard operator would arrive at his post at six in the evening and settle in with his hi-fi and chess set. The switch board was situated with a window overlooking the hospital entrance and so the switchboard operator saw everything and everybody who came and went.
Doctors would often play him a game of chess late at night and of course he had a feel for what was happening in the hospital and how urgent things were. All phone messages from the hospital came through the switchboard. He could tell by the urgency in the voice, asking for example to be put through to the pathology laboratory or to the duty consultant that urgent and sometimes critical procedures were going on. If Sara phoned to ask what was happening, he would say “Mr Maybury is just finishing an operation and should be home soon,” or “I think Mr Maybury is in the middle of a difficult procedure and may be a while.” When I did get home Sara would have tea ready and as always we caught up with the day’s events before turning in for the night.
We frequently had company at mealtime. One friend and colleague who visited was Julian Sansom, the surgical registrar at Stratford-upon-Avon hospital
Julian and I covered emergencies at each other’s hospitals when the other was off duty. One hot Sunday in summer I was called over to operate on a patient who needed an urgent laparotomy at Stratford-upon-Avon Hospital. The hospital straddled the cattle market in the town, so the patient had to be wheeled by trolley across the entrance to the cattle market to reach the operating theatre. It was very hot in the theatre, which did not have air conditioning, so I asked for the window to be opened and a cool breeze brought relief.
After a few minutes there was a shout from the anaesthetist and looking up I saw a cow was staring at us having stuck her head through the open window. The cow was shooed away and the window closed leaving us with three or four flies wheeling round the operating theatre light. Quick action was needed before they contaminated the open wound. Fortunately, the anaesthetist was resourceful and filled a syringe with ether and placing the finest needle onto the syringe used it to kill each fly in turn with a well-directed squirt of the anaesthetic agent. All the flies were so dispatched and there was no contamination.
One morning the Firm headed by Mr Marsh was doing a ward round and we came to a patient who had problems swallowing and a barium X-ray had shown her to have a very long growth of the oesophagus. We had moved away from the bed and were discussing what could be done, then Mr Marsh decided a Moussin-Babin tube should be pulled through the tumour to enable the patient to swallow liquids. I suggested a radical resection. Mr Marsh looked at and with a slight smile said, “Now you are a registrar you are entitled to an opinion, I have considered it and we will do it my way and gave his reasons.
I appreciated this approach because he had allowed me an opinion, then thought about what I had said and had not changed his mind. Next day at the operation he was obviously right as the cancer could not be removed, so we pulled the tube through the narrowing of the oesophagus.
Several years later I was assisting one of my chiefs at an operation, when it seemed as though he might be about to make a mistake, I said. “Do we mean to do that Sir”. To which he immediately replied, “Just testing!” and changed what it appeared he was about to do. I do not know if I saved the day or if he was seeing if I was concentrating, either way it was a good lesson.
When a consultant I always encouraged my registrars to have their say, which I always considered carefully, because occasionally decisions have to be reversed or revised due to changed circumstances or technological advances. Jokingly explaining to them that if a patient said; “Mr Maybury said you were to take off my head. You must query the decision before acting”. Usually the considerable experience of the older surgeon, in what is after all a craft, held sway and was proved right, but it gave the opportunity to change course and no patient ever had the wrong operation.
Mr Marsh often quoted ‘bon mots’ to me. In my book, “The End of the Golden Age of General Surgery1” is described an operation I was carrying out in the twin theatre next to the one where he was operating. There was haemorrhage and I asked the nurse to go through to Mr Marsh to ask for help. I heard him loudly say, “Let him sweat for a bit”. I did not hear the rest of the sentence but the nurse came back and told me that Mr Marsh had said, I was to put a pack into the operating area and he will be along soon. This I did and he came and showed me how to sort the problem out, so then I would know what to do the next time.
From this I learned two lessons. The first was that if all operations proceed smoothly I would never learn how to solve operative difficulties for the future safety of patients. Mr Marsh carried out many technically difficult operations at which I assisted and learned This is the inestimable advantage of the true apprenticeship, seeing the chief most days and assisting him on these occasions during four lists a week, in a calm atmosphere with continual discussion of all things surgical related to our patients. This was in addition to the lists I did myself.
The second lesson was rapidly learned, that if the going was difficult to stay calm and think logically and call your chief before doing anything damaging. Anxiety is inevitable in the profession and at times the pulse races.
In the seventies, recordings of the changes in the pulse rate of surgeons during operations of different complexity was studied. The results were interesting in that, even during simple procedures by an experienced surgeon, the pulse rate rose, while during difficult major procedures the pulse rate would soar. Therefore, controlled anxiety was the norm. Mr Marsh said he would not trust a surgeon whose pulse rate did not rise while operating.
He took me down to London to attend a conference and afterwards gave me some advice. People presenting work at conferences always produce their best x-rays and graphs. If you really want to find what is going on find the speaker’s registrar in the bar afterwards and see what he has to say about his chief, adding rather cynically that no surgeon is a hero to his registrar.
During my two years as Mr Marsh’s registrar, I was taught and then carried out a large variety of operations. Including the closure an open spina bifida, in a new born babies who was leaking cerebro-spinal fluid (CSF) due to this exposure, making infection of the lining of the spinal cord and brain likely if not closed. In the first half of the twentieth century and earlier these babies did not survive. The condition can be accompanied by incomplete development of the brain and spinal cord and in these cases surgery was not carried out.
Following the operation there is often a build-up of pressure in the brain which will result in hydrocephalus due to enlargement of the CSF filled ventricles of the brain which in turn enlarges the head due to separation of the skull bones which are not fused at this age.
To prevent this occurring I was taught to insert a Spitz-Holter valve to drain the excess CSF from the brain via a tube run under the skin into the peritoneal cavity in the abdomen. These were satisfactory operations. Occasionally the valve which only allows the CSF to flow from the brain into the peritoneum and not backwards became stuck. It could usually be reactivated by pressing on the valve under the skin of the neck.
This experience of cranial surgery was augmented by looking after many serious head injuries from traffic accidents who were brought to the hospital being the only accident centre in South Warwickshire and at that time there was only one surgical registrar at the hospital and that was me.
Many times I placing six burr-holes in the skull of a road traffic accident patient, to search for and if present to drain a sub-dural haemorrhage. These operations could also necessitate raising a cranial flap or elevation of depressed fractures of the skull as necessary. There were no scans in those day so the decision to operate was taken purely on the history and careful examination alone. There were skull x-rays but these cannot diagnose intra-cerebral haemorrhage or oedema.
It was always very important to speak to the ambulance men who brought in the traffic accident victims. On several occasions the ambulance men told me that the patient was talking when they arrived at the scene of the accident and now before me was a deeply unconscious patient.
There patients clearly had a functioning brain immediately after the accident, so subsequently something had happened inside the skull to render them unconscious. Essentially there one of two reasons or both. They had either had an intra cerebral haemorrhage and or catastrophic cerebral oedema, this latter is rapid swelling of the brain, the cause of which is still not fully understood. If the cause was haemorrhage then there was a chance that surgery would help, if oedema was the cause of the deep coma then these patients were unsalvageable and would die.
On clinical diagnosis it was not possible to differentiate these events, so all these patients were taken to the operating theatre with a view to placing the six burr holes in the skull with and an added craniotomy if needed should haemorrhage be the problem. In many patient’s haemorrhage was the cause of their loss of consciousness and evacuation of the blood-clot, on one or both sides of the skull gave the patients the best chance of a full recovery. Unfortunately, if on placing the first burr hole the internal pressure on the brain was so great that brain itself exuded through the burr hole, then there was nothing further to be done. I would then go to speak to the relatives who were naturally shocked by the accident and needed as gentle handling as possible, but had to be told the dreadful news.
Some surgeons feel guilt at this point that they could not do more. If everything had been done, that should have been done, then I could speak to the next of kin calmly without angst. I felt sorry for them and explained slowly, allowing the relatives to speak freely, while telling them of the terrible outcome of the injuries. Then if they wished, going through what was known of the accident, the diagnosis, the operation findings and their tragic and unhappy significance of brain death. In these circumstances, when there is no hope of recovery, the relatives must understand this, however long it takes to gently explain. These explanations also help the doctors and nurses who need to look after the patient during the brief time until death occurs.
For a very short while I toyed with the idea of being a neuro surgeon, but decided against. I enjoyed urology and was not put off by abscesses full of pus or other infections or the malodourous contents of surgery on an obstructed colon. I was firmly focused on the prospect of being a General Surgeon, even though the training was the longest of all the then specialties. On average trainee general surgeons were being appointed as consultants at on average forty years of age or more, but were rewarded by a wide variety of interesting work1.
Just before we left Warwick on going to the local fish and chip shop to buy supper, a nurse was also waiting to be served who had on a number of occasions baby-sat for us. Then to my surprise another identical young woman came in. I had never known that Rose had a twin and on chatting to them discovered that they had both baby-sat for us, they were the most identical of identical twins that I had ever seen with exactly the same voice and as far as I could gather they had shared the job of a single nursing post as well as the baby sitting. We all had a good laugh at my ignorance for not knowing and not noticing.
To complete the job requirements to ensure broad experience before being eligible to sit the examination for the Fellowship of the Royal College of Surgeons (FRCS), I switched to be the orthopaedic registrar at Warwick Hospital for a few months and then took a fortnight’s holiday. The first holiday since starting work in Warwick. This quiet fortnight in Sussex reading for my examination served me well and a short time later, the examinations behind me I was elected a Fellow of the Royal College Surgeons of England. The date was 1972.
While at Warwick I learned the craft of surgery from John Marsh, it was the best of jobs. Now I was advancing, in the surgical sense, towards becoming, “All things to all men1”, at a rather earlier stage in my career than anticipated.
Reference:
*The End of the Golden Age of General Surgery 1870-2000. The Training and Practise of a General Surgeon in the Late Twentieth century. Publisher: Createspace. 2015 ISBN 1499531370. Ch. 2. Page 11. Available on Amazon.
CHAPTER 5: Back in London.
I had applied for the job of Post Fellowship Registrar at the Middlesex Hospital*, which was next to Soho in London. The post of surgical registrar was advertised to work for Mr Cecil Murray and Mr William Slack, later knighted, who were the consultants of one of the general surgical firms with a particular interest in endocrine and colo-rectal surgery respectively.
On entering the imposing lobby of the hospital I noticed a beautiful Queen Anne table** in the centre which was deeply inlaid. The table was generously proportioned being about eight feet across with a splendid pedestal support. It had a magnificent bowl of flowers in the centre which were daily refreshed by the Friends of the Hospital.
I asked the porter for directions to the interview room and found the waiting room already occupied by a number of other candidates some of whom I knew. My spirits dropped but I did not allow it to show and was much surprised after all the interviews had taken place to be called back in and offered the job. I accepted with pleasure and was expected to start work within a month.
Sara put our house in Warwick on the market and were kindly invited by friends of my wife’s parents to stay once again in their Oast-house next to Brightling Place, in Sussex.
Life for the next three months at Brightling Place could not have been better. I caught the train from Robertsbridge every weekday while Sara enjoyed her days at the Oast-house. It was while we were living there that it snowed heavily and for the first time in my working life I could not go to work. For three days the snow was so deep that the road to Robertsbridge Station was impassable, making it impossible to catch the London train. I felt very guilty about not going to work but it could not be helped and I enjoyed the time at home.

One weekend during our stay in the Oast house we went to London to look for a house to buy. In the Evening Standard that Friday evening there was an advertisement for a small terrace house in Bellamy Street in Wandsworth. At that time the housing market was overheated with rapid price inflation and there was now a house buying frenzy. Knowing that speed was of the essence to secure a property, I immediately drove over to see this house. It was a tiny two up and two down Victorian house, built probably in the eighteen-eighties in a long terrace sweeping down a hill with a matching terrace on the other side of the road. It was charming and at the back was a garden seventy feet long with a splendid silver birch tree and flower beds overflowing with roses which grow so well on London clay.
On entering the house, I found that there were already four couples there looking around. There were no cell phones in those days so I left immediately and rushed back to collect Sara and half an hour after leaving the house we were both looking around the house. There were still four couples in the house looking around. It took Sara about two minutes to decide that this was a house we could live in and enjoy. Quickly finding the owner we immediately offered to buy the house at the asking price and gave him a cheque for ten percent. The price was eleven thousand pounds. We had taken advantage of knowing about this buying and selling frenzy in the housing market and a few days earlier had arranged a mortgage in principle and a loan for the deposit from the building society.
With cheque in hand the owner accepted our offer and the deal was done. Sara and I had never taken more than a few minutes to agree on all our major purchases in life. We were very pleased with the house and some two months later the purchase of 42 Bellamy Street in Wandsworth was complete and became our favourite house. No survey was done but as all the houses the street appeared to be in a good state, all having their original slate roofs with no evidence of sagging or cracking of the brickwork. Perhaps the most notable thing was that the house was affordable and the mortgage needed was less than three times my salary. This was insisted upon by the mortgage company and evidence had to be presented that the salary quoted was real by having a payslip scrutinised. We left the Pepys’s with great regret but were excited that we were moving into a house of our own again.
Before the Second World War Bellamy Street had been a street of artisans with their families. Our next door neighbour, who had lived in the street from that time, told us that the street used to be bustling with activity, while the men were out at work their women folk were busy about their daily life, which included socialising, popping in and out of each other’s houses, while the children played in the street. Now twenty-five years later, in the early seventies, the street was empty during the day.
The nearest underground station was Clapham South on the Northern Line, only a short walk away and took me directly to Tottenham Court Road Station in central London. This short journey often took over an hour due to the overcrowding and irregularity of the trains in those days. The walk from the house to the tube was initially depressing, due to rubbish and dog waste on the pavements. After a few months I had stopped noticing these unpleasant intrusions into daily life and got used to reading on the tube either sitting, a rarity, or standing.
In Warwick I had been on duty virtually all the time, but lived at home one hundred and fifty metres from the hospital and went home if there were breaks in the work. The Middlesex Hospital being in the centre of London was very busy by day, but as all the commuters left for home it became very quiet, with very few emergencies for the duty surgeons to look after or operate on. It is a truism, that when there is little to do, the inclination is to do less. So any emergency was more of an effort to get on with. The surgical registrar rotation was that I lived in the hospital one week in four.
However, my time was well spent at the Middlesex. My reading of surgery deepened and there was time to consider diseases and operations in depth, with regular clinical seminars and attendance at medical conferences, especially the Association of Surgeons and the Surgical Research Society. It was an enjoyable time in a very different way from the total absorption with continuous operating lists and emergencies. A slower pace now with more contemplation to redress the balance in my training, but at the expense of some boring times when resident in the hospital, with little in the way of emergencies to look after. Even this gave me the time and opportunity for more reading which I gladly took. The surgical disciplines in which I had the opportunity to advance at the Middlesex Hospital were endocrine and colorectal
One weekend at Brightling, we were introduced to Dr and Mrs. Wimbush, a charming elderly couple. In the course of conversation, Dr Wimbush told me that he had been the last Medical Superintendent of the Hammersmith Hospital which became the first post-graduate Medical School in London in the fifties. In those days the administration of the Hammersmith Hospital consisted of the Medical Superintendent, the Hospital Secretary who answered to the Medical Superintendent and the Officer of Works. There were two secretaries and a handful of other personnel. Dr Wimbush was himself a full time Consultant Physician. He exercised all his duties of administering the hospital between eight and nine o’clock every weekday morning and for the rest of each day attended to his medical duties. He told me that he was not paid for his management role. This was an interesting insight into administration in the immediate post war period. Management only appeared, years later, when financial responsibility was taken away from the consultants and over time lead to the birth of regulation and ultimately targets, all with malign consequences.
The end of my appointment at the Middlesex, which was for two years, was now in sight and I was wondering how to pursue my career. As already mentioned there was no set pathway to become a consultant general surgeon in the seventies.
I was interested in immersing myself in research, to experience the excitement of being a scientist and break new ground for a while. In 1975 I was awarded a Wellcome Trust Research Fellowship following a long and detailed interview, as a result of which I received a two-year grant. This was to work in the Academic Department of Surgery at the Middlesex Hospital under the supervision of Professor Michael Hobsley.
I was to study the efficacy of surgery in curing duodenal ulcers, with hopefully revealing how to improve the operative success rate. This was a daunting task as the success of curing duodenal ulcers by surgery was 93%5. The interest in this disease in the seventies was that it affected ten percent of the population at some time in their lives and often ran a long course over many years relapsing at intervals and causing the loss in nineteen-seventy-three, for example of one-million-eight-hundred-thousand working days in Britain. Surgery was largely reserved for those with debilitating chronic disease and in the seven percent in whom the operation failed to cure the ulcer, the aftermath of the surgery could be serious and chronic. The results of the research are described in detail in “The End of the Golden Age of General Surgery3” published by the author in 2015.
One day, on arriving home after spending the day on my research, Sara told me that Dr Horace Fitzpatrick had phoned. Fitz as he was known was the American husband of Sara’s cousin. He was a professional musician and at that time a Visiting Professor of the Natural Horn at the Guildhall School of Music. He told Sara that his most brilliant student had been knocked down by a red double-decker bus. He was very worried about Peter who had been admitted to St James’s Hospital in Balham as an emergency three days earlier. Fitz thought Peter looked ghastly and would I please go and see him.
Forthwith I went to St James’s Hospital and soon found Peter on a surgical ward. He was as white as a sheet and very weak. I introduced myself and asked if he minded me examining his abdomen. I am normally a stickler for correct etiquette, but Peter had been languishing on this ward for three days and told me that no operation had been proposed. This looked to me a desperate situation and was no time to stick to medical etiquette. Looking at him from the end of the bed he obviously needed a laparotomy and probably had a ruptured spleen. On examination his abdomen was tender and full of fluid, which was obviously blood, Peter’s blood pressure was low although he was cerebrating and passing urine.
Having completed my examination and feeling very concerned about this young man I went to speak to the Ward Sister. She confirmed that no active treatment had been planned. I explained who I was and asked if I could speak to the duty surgical registrar. The Sister immediately acquiesced, as she was worried about Peter too, and to his credit the registrar came straight away. He had not seen Peter before as he was not one of his chief’s patients and agreed that we go to examined him together. The Registrar confirmed that the likely diagnosis was a ruptured spleen and immediately arranged to cross match several pints of blood. He then spoke to his chief who advised immediate surgery. Feeling much happier I left for home as I did not wish to outstay my welcome.
I rang St James’s next morning to enquire about the patient, to be told that he had had his laparotomy late at night and indeed had a ruptured spleen, which had been removed. He was recovering well and already feeling much better. In those days one could find out what was happening just by asking. I dropped in frequently to see him and after three weeks Peter was ready to be discharged to his lodgings in Streatham.
His landlady would only provide him with bed and breakfast. We could not put him up in our tiny house in Balham with only two bedrooms and two very small children. Sara had a brilliant idea. Every morning after breakfast, Peter who was still very weak but otherwise making an uneventful recovery was able to take a taxi to our house, where Sara looked after him and fed him. We would all have supper together when I got home in the evening. I would then drive him back to his lodgings. Peter’s parents came over from Connecticut to see him and to my horror his mother fell from the back of a London bus but fortunately was not seriously hurt.
This pleasant routine continued for several months until Peter was fit enough to start playing the horn again, which he did in the shed at the bottom of our garden. He returned to the Guildhall to finish his course and afterwards went back to the United States. We had become good friends and we met again a few years later when we visited the States. He gave the boys catapults and more delightfully showed them how to make ice cream in a hand turned churn. Now as I write Peter is Professor of the Natural Horn at Eastman College in New York, arguably the most prestigious school of music in the United States.
While visiting St James’s to visit Peter I had usually entered the hospital through Casualty and noticed that sometimes it was closed in the late afternoons and evenings. I rang the personnel department who were delighted to accept my offer to man the department when they were short and would otherwise have to close it. It worked out that I was the sole casualty officer on average twice a week from six pm to midnight and this I enjoyed immensely. As Sara said it stopped me wanting to operate on the dog.
When on duty in St James’s all patients who came to casualty were seen by me. It was extremely busy and once more I had trauma to diagnose and treat. This gave me the opportunity to set fractures on the one hand and see all the patients with acute abdomens sent in by the General Practitioners on the other. This last group were of great interest to diagnose and start resuscitation as necessary, while bringing these patients to the notice of the duty registrar. It soon became known by the GPs that a “Tommy’s” man was on duty in the evening at St James’s Hospital and this precipitated the referral of many patients with acute back pain. After examining them and taking x-rays of the spine they were referred to Dr Cyriax3 chief of the Physical Medicine Department at St Thomas’s for urgent manipulation, following the programme I had learned in Casualty at St Thomas’s. It was a pity but St James’s Hospital was closed a few years later in 1998.

When the term of my Wellcome Trust Fellowship had only six months to run the search for the next job was started. For career progression the next appointment must be as a Senior Registrar the last stage before being eligible to apply for a Consultant Surgeon’s post. Looking for a new job was interesting but not straight forward, as surgical training was carved out by the individual aspirant as opportunity and capability allowed.
To my surprise I was headhunted for a job at a University Hospital outside London. I went to have a look. It was a fine place but as I was taken round it became apparent that the role of the holder of this post of Lecturer in Surgery/Senior Registrar must have considerable operating experience, above that of the average, which thanks to my time at Warwick and the Middlesex Hospitals I had.
The reason this was desired was initially obscure to me, but it gradually dawned that the Professor was often absent. This was not in itself unusual, as busy Professors often had wide and sometimes international duties to attend to, but in this instance the need appeared to be due to a problem the professor had with alcohol. It would be flattering to take on many of the duties including operating for the chief, which if this was the case would protect the patients, but it seemed unlikely that I would learn anything new and so I would not be better placed for a consultant post in four years-time when I would be eligible to apply for one. I declined to apply for this post which caused considerable consternation back at the Middlesex until I explained my reasons to my chiefs. I did notice that the professor in question retired shortly afterwards.
The next job I looked at was in Cardiff. It was a lovely hospital and job. However, on arriving at Cardiff Station I was greeted with writing six feet tall on a wall at the station which was quite straight forward, it was just; “Go home English”. There was a strong undercurrent against the English at the time. This was something I was not willing to submit my family to, especially considering that schooling for Nick had been so atrocious when we were living in Balham, so I did not apply.
By now my contract as a Wellcome Trust Fellow was running out and looking for a senior registrar post had become urgent. A post in the Professorial Unit for a Lecturer in Surgery was advertised at the new Medical School in Leicester. The appointment attracted me and I applied.
Sara came with me to Leicester to look round the town to see if she could find an area in the town where it would be pleasant to live. I went to the interview while she went searching. Later that day we met at a prearranged rendezvous and the first thing she said was; “I hope you have the job as I’ve bought a house”. I had been appointed as the new Lecturer in Surgery/Senior Registrar and so we went happily to view her purchase.
The house was a splendid large Edwardian semi-detached house with five bedrooms, a large sitting room an equally large study with the original moulding on the ceiling. The house also had a cellar. The garden was small but walled and contained a period listed greenhouse in some disrepair. The man of the family selling the house was himself a lecturer at the university and was moving to another university so vacant possession was only a few weeks away.
The house that we now sold in London was an end of terrace in Lynette Avenue, a road off Clapham Common. Eighteen months previously we had moved in, having found our favourite little house in Bellamy Street just too small with two growing children. We had sold it for twelve thousand pounds and bought the new house with a view to doing it up to make some money. Within a few weeks the kitchen was stripped out and converted into a lovely kitchen diner with pine wood furniture which was all the fashionable rage at the time.
By the time the Lynette Avenue house was finished it was time to move on. To sell this house we placed an advertisement in the Sunday Times for two consecutive weeks only. House buying fever was in the air again and this meagre advertising sold the house within a week, thus avoiding an agent’s fee and we made a small profit out of the fifteen thousand we had received for it. The funny thing was the original fireplace in the sitting room had a beautiful moulded but separate over-mantle which we had carefully restored. It was this that our purchasers fell in love with and insisted it went with the house. So an over-mantle sold the house for us for fifteen thousand pounds.
*The Middlesex Hospital and Medical School was finally closed in 2005, as all the departments including surgery had already been absorbed into University College Hospital. It had been founded in 1745 on Windmill Street and moved to Mortimer Street in 1757. It had been a teaching hospital for nearly two hundred and sixty years.
**The Queen Anne table in the main Hall of the Middlesex Hospital was stolen a few years later. At seven o’clock one weekday morning a large van drew up in front of the hospital and two men in white coats entered the hall and asked the porter to move the vase of flowers as they had come take the table for repairs. That was the last time it was seen which was a great shame.
***The End of the Golden Age of General Surgery. 1870-2000. The training and practice of a General Surgeon in the late Twentieth Century. ISBN 1499531370 and 13: 9781499531374 (Published by CreateSpace, 2015). Available on Amazon. P. 44-53.
CHAPTER 6: Return to the Midlands.
Professor Peter Bell, later knighted, was my de facto chief as I was a lecturer in Surgery in his department. He a good chief to work for and he taught me a great deal about surgery, and from him I learned vascular surgery. He was a brilliant surgeon and teacher. He liked informality and everybody called him Peter.
He was one of the founders of the Vascular Surgical Society which flourished, but he was a bit disgusted that one of the first acts of the Society was to order a magnificent chain of office for the Society’s President which he considered quite unnecessary. He proposed me for membership of the society, for which I was grateful, and for many years I regularly attended the meetings which met in different cities and on one occasion in Ireland.
On the final evening our Irish hosts gave a splendid dinner in an ancient hospice outside Dublin. The meal was excellent and the after dinner speeches were the funniest that we have heard. The final speaker ended by saying in a very hoarse voice that the Irish were a nation of tired speakers and no listeners.
One weekend the whole family travelled to Steeple Aston in Oxfordshire where the Fitzpatrick’s lived. Dr Horace Fitzpatrick, known to all as Fitz was introduced in a previous chapter. Our car broke down and Fitz offered to lend us his hearse, an ancient Austin Princess that he used for carrying large tree trunks, which were the raw material for the musical instruments he made. These were Serpents and Gems-horns, medieval musical instruments which he produced with consummate craftsmanship.
Thus we arrived back in Leicester in the magnificent old hearse. My wife and I in the front and our sons further back on either side where pall bearers sat. It caught the eye of the public where ever we went but was also a devil to drive. The foot brake didn’t work. To stop the hearse, it was necessary to haul the handbrake on forcibly, which made the vehicle slew to the left, to counterbalance this it was essential that the right hand was engaged heaving the steering wheel to the right to ensure the hearse did not swerve and kept moving forward in a straight line until it stopped. This was heavy work as there was no power steering. We used this hearse as our car for some months.
I worked for Mr Bolton-Carter for six months as his Senior Registrar and learned a great deal of thoracic surgery, especially lung and oesophageal resections. One day he was in chatty mood and told me that his father had been the first general surgeon to work at the Royal Infirmary shortly after World War I, adding that his father had earned six thousand pounds in private practice in his first year as an Honorary Consultant without pay at the Royal Infirmary, a considerable sum of money in those days.
It was Horace Fitzpatrick’s hearse that I parked outside casualty when I had hurried down to the Royal Infirmary to operate on a man who had been stabbed in the heart1. I opened his chest and the pericardium surrounding his heart to close the stab wound in the left ventricle. The patient survived the operation and went home six days later. This was an example of the charge against the assailants being reduced from murder to grievous bodily harm as a result of modern surgery. The next day I was mildly admonished by Mr Bolton-Carter for backing two horses at once by operating while keeping a hearse ready outside!
On Wednesday afternoons there was a list of straight forward operations such as repairing inguinal hernias and stripping of varicose veins in a small day hospital just a few yards up the road from the Royal Infirmary. Not infrequently I would find myself operating with a very senior anaesthetist who was not so far from retirement. The hospital was quiet, a pin could be heard dropping in the operating theatre and over a few weeks the anaesthetist and I got chatting. After some weeks it seemed appropriate to ask his advice about a career in the NHS. “What is it like to be a consultant after years and years of training?” He replied para-phrasing Shakespeare; “Well my boy, think of it like this. Ripen, ripen, ripen then rot, rot, rot.” Then he threw in some gratuitous advice: “You may find out that an NHS salary is not enough to keep a mistress!” I enjoyed those quiet afternoon lists but he never enlarged on his second remark!
It was in Leicester that I looked after head injuries again and operated on patients with subdural haematoma on the brain. The difference from Warwick in the management of head injuries at The Royal Infirmary was that a CT scanner (computerised tomography) was available and to which all severe head-injuries were sent for a scan. No longer were operations carried out by relying on a clinical examination alone. The outcome was that thanks to the CT scan we did fewer operations, as those unfortunate accident victims, who had irremediable massive trauma to the brain, could now be identified by scanning. Artificial ventilation could now be turned off once their relatives had come to terms with the inevitable outcome of their trauma.
The scan in another patient might identify a unilateral subdural haematoma that would only require one well-placed burr hole in the skull to evacuate it, rather than the mandatory six when operating before the days of the modern scanner so as to avoid missing a contra-lateral haematoma. Now there was also the technology and means of inserting a pressure monitor probe through the burr hole and placing it between the skull and dura, the tough outer lining of the brain. If the pressure in the skull went up, then a new CT could be carried out to assess whether further surgery would be useful. It was good that the surgery was more focused, but the most pleasing fact was that in the days of clinical assessment only, we had not been missing patients who would benefit and should be operated on.
It was in Leicester that I operated on a one-year-old infant with a rapid loss of consciousness due to the rare intracranial extradural arterial bleed after fall out of his pram. This is caused by the middle meningeal artery being torn. As the infant rapidly lost consciousness with a dilating pupil he was immediately taken to the operating theatre suite and I drilled a single burr hole over this artery and clipped it above and below the tear after evacuating the clot. It is one of the joys of surgery to be able, in this case, to tell the mother that her son was conscious and all would be well.
I started looking for a consultant post in the autumn of 1979. I had been a Lecturer/Senior Registrar for two and a half years and was appointed six months later as a Consultant General Surgeon at the Royal Albert Edward Infirmary in Wigan in the North-West Region in England. Once more Sara was selling our house and looking for somewhere to live.
Reference.
*The End of the Golden Age of General Surgery 1870-2000. The Training and Practise of a General Surgeon in the Late Twentieth Century. 2015. Publisher Createspace. ISBN 1 499531370. Chapter 8. Amazon and Kindle.
CHAPTER 7: Move to the North West.
Coccium is mentioned in the Antonine Itinerary, which was a second century map thought to have been drawn for the Emperor Antonius Pius and was built on a Roman Crossroads by the River Douglas en-route to the north and Hadrian’s Wall. It is thought that the Romans mined the land on which the modern town of Wigan is built. In the Middle Ages Wigan was a pleasant town and one of the four Royal Boroughs in Lancashire. Apparently at the end of the eighteenth century it was a spa town. Seams of coal under the town have been mined since the middle ages, this picked up pace in the Victorian era resulting in the centre of the town being covered with gigantic spoil heaps. These still covered one hundred acres in the very centre town when I took up my post at the Royal Albert Edward Infirmary as a consultant general and vascular surgeon.
There is an interesting piece of folk law which I heard but am unable to corroborate, that before the nationalisation of the coal mines in nineteen-forty-seven the pits in Wigan which are on Church land brought in considerable revenues. The Bishop of Liverpool in whose Diocese since eighteen-eighty All Saints Church has been situated was reputedly the richest Prelate in England, he was also the Rector of Wigan and in those far off days always appointed a curate in charge.
The huge area of spoil tips in the centre of town were very much in evidence when my wife and I and our two sons arrived in Wigan in the winter of nineteen-sixty-seven to have a look at the town after seeing the post for a consultant general surgeon advertised.
Another remarkable feature of the town is Wigan Pier. It exists and is well worth a visit. It is the pier for the Leeds Liverpool Canal and as Wigan was one of the greatest coal producing towns in the nineteenth century, barges were the means of transporting the coal to Liverpool from where it could be shipped on. The Pier was made famous by George Orwell in his book “On the Road to Wigan Pier” and has become so popular that by the end of the twentieth century it attracted a third of a million visitors a year. Well worth seeing the ingenious mechanism of emptying the coal brought in waggons from the collieries into the barges made famous by George Formby in one of his songs.
Overall is spite of its interesting past Wigan was very run down as a town when we first visited. It had not been badly bombed during the Second World War so it had escaped the horrors of post war nineteen-sixties buildings which had hideously replaced the centre of badly bomb damaged St Helens for example. In Wigan the old and dilapidated covered market still existed and the one-hundred-acre centre of the town consisted of spoil tips from the old coal mine.
I visited the Royal Albert Edward Infirmary (RAEI) for a prearranged tour. Much of the old building including the entrance and some wards were still as they were when Prince Albert Edward opened the building in eighteen-seventy-three. The Out Patients were in pre-fabricated huts built in World War II, despite this the old buildings had a good atmosphere and the nurses were smart and the patients appeared well looked after. There was a suite of two interconnecting operating theatres, pretty well identical to those I had worked in at St Thomas’s in London and Warwick Hospital. There was simple sparse Intensive Care Unit. I thought that this would be an interesting challenge and after discussion with Sara put in an application. Following the interview, I was appointed to start work on All Fools Day nineteen-eighty.

Meantime my wife was searching for a house to buy in Wigan after putting our comfortable five bed-roomed semi-detached house in Leicester on the market. Our luck was in as the Leicester house was almost immediately bought by an architect who had always wanted to own one of these houses of which there are only four in the city. Since only one buyer is needed and he was willing to pay the asking price we now had the means to buy a house near the hospital.
The rules stated that a consultant must live within a radius of seven miles from his or her hospital, so emergencies could be reached easily and quickly. In Wigan there were relatively few pleasant town houses for sale, or at least none on the market, so a search for a new house was started and we were lucky to find one just in the process of being built in the village of Standish.
Unsurprisingly most Britons have never heard of Standish while many Americans would know the name because Captain Myles Standish had sailed in the Mayflower to America in sixteen-twenty. In the early part of the twentieth century Standish Hall in Standish was bought and transported brick by brick to the USA where it was reassembled (1).

The original village had now grown into a pleasant dormitory town contiguous with Wigan. Sara found Standish, in the same way she had discovered Stoneygate where we had lived in Leicester. This was by asking ladies at a bus stop in the centre of town, where did they think the best place to live would be if they had the choice. Such a straw-pole taken one afternoon came down heavily in favour of Standish. So that was where we went to look.
The builder of the house we had our eye on was also the owner of the building company. He told me that he only wanted to deal with me. I answered that my wife knew infinitely more about houses than me and would make all the arrangements including purchase. He was rather flabbergasted by this, to him, unsatisfactory arrangements but was quickly brought on side by Sara and all went well.
Our new house had had the foundations laid. The site overlooked a small valley with a stream in which later our sons spent many hours playing. Beyond there was an excellent view of Winter Hill in the distance, a splendid landmark which when travelling north on the M6 and on crossing the Manchester Ship Canal, thirty miles to the south, could be seen in the far distance dominating the landscape, often capped with snow in winter. In due course travelling north and seeing Winter Hill meant we were nearly home.
Further down the valley was a large spoil tip, the last remains of Victoria Colliery which had only recently closed. The slag on the tip was rich in fossils of the carboniferous period which Nick and William collected. Within the next few years all the coal mines in Lancashire closed. It was indeed the end of two millennia of mining in that part of Lancashire. In spite of the closure I treated many miners in my first few years of practice there.
While the mines were closing the last of the cotton mills also closed. It was interesting to see and hear older women, who had worked in the noise of the mills “me-mawing”, speaking with accentuated lip and mouth movements, so they could chat while at work. This way of speech was copied by the daughters of these women even though they had never worked in the mills themselves.
The house was not due to be finished for some weeks after our arrival, so giving us the opportunity to alter some of the room plans. Reducing the size of the large sitting room allowed space for a study cum consulting room, useful if I should be referred any private patients. We also slightly reduced the size of the master bedroom so the fourth bedroom could be enlarged giving the house four double bedrooms.
A few weeks later, in the driest and dustiest April anyone could remember we moved into our new house. As with our first house in Gillingham we were the first occupants of the development. The house was big and comfortable. Cranleigh, the name of the road, was tarmacked but in the winter of nineteen eighty it snowed very heavily and repeatedly for six weeks, since ours was the only car using the road, it looked as though it would soon be impassable. With great difficulty I drove the car to the top of the hill where Cranleigh joins the main road. Fortunately, this was before the snow had become too deep so I parked it near the main road. Some days when I reached the car from home I was able to use it, but on many occasions the main road was so treacherous that I walked the three miles to the Infirmary in the snow.
At Christmas it was normal to work on Christmas Eve and have a list of minor cases. Following Boxing Day, work continued as normal including full lists with major cases with only the New Year’s Day bank holiday as respite.
We soon got into the rhythm of life which was in many ways hum-drum. My wife managed my private practice and over time gradually got to know all the GPs as they were happy to arrange appointments directly with her, often she thought that their patient being referred was in the GP’s consulting room at the time. It was busy at the Infirmary and I had six operating lists a week until nineteen-ninety-nine. Private Practice took a small portion of my time, about ten percent, and I arranged a part time contract with the National Health Service which permitted me to practise privately in exchange for a reduction of ten percent of my NHS salary.
From the inception of the NHS in 1949 and some years thereafter many GPs in the provinces doubled as surgeons at the local hospital, carrying out mainly minor and intermediate operations, everything more complex went to the teaching hospitals. Those patients who were referred to the teaching hospitals were the very patients on which the new generations of general surgeons were taught during their training in the 1960’s and 1970’s. As these surgeons were in time were appointed as consultant general surgeons to District General Hospitals the necessity of sending patients back to the teaching hospitals declined to a mere trickle. I belonged to this last generation of general surgeons who were so trained, when I was appointed to the Royal Albert Edward Infirmary in Wigan.
Before the interview I discovered on my visits to the RAEI that no vascular or oesophageal surgery was carried out and there were no specialist surgical instruments in stock. As a member of the new Vascular Surgical Society I had access to a national survey of vascular operations performed across England and from these figures it was apparent that about forty major vascular operations would be needed for patients in the RAEI catchment area while before nineteen-eighty there were none. I estimated that there would be sufficient time on my operating lists to accommodate this number of major vascular operations annually.
Armed with this information, I set out from the date of my appointment in January nineteen-eighty to acquire the necessary instruments to carry out vascular and oesophageal surgery before starting work three months later on the first of April 1980. This was successful and is fully described in The End of the Golden Age of General Surgery**. Thus from the day that I started work as a consultant surgeon the operating theatres were equipped and ready for this type of surgery as and when patients were referred by their GPs.
I was pleased to be in position to provide these services locally from day one. At that time, it was easy to make such arrangements and I felt that the changes needed to achieve this had to be in place before starting work as a new consultant, for if they were delayed then inertia could overtake the process and nothing would change.
Therefore, it was fortunate that no business plan or management permission was required to set up this new service. The wide range of skills I had learned during training had been discussed at the interview and this was taken as a green light to go ahead. Naturally these matters were discussed with my new colleagues and they were kind enough to give me encouragement. As a result, during the rest of 1980 nine elective major vascular operations were carried out and this increased to over fifty annually including emergencies by 1995 (2).
In the early eighties it was common for GPs to request a consultant to make a domiciliary visit to see a patient. On my first day as a consultant I was asked to see a boy of seven with acute abdominal pain at his home. He had a complex history due to severe cerebral palsy and as a young baby had a Spitz-Holter Shunt inserted into his cerebral ventricles to permanently deliver excess cerebro-spinal fluid into his peritoneal cavity (3). He had previously undergone several abdominal operations and was once more suffering from abdominal pain. The GP’s was asking whether the child should be admitted or could he be treated at home?
When I examined him, the poor child had an abdomen like a drum and clinically the diagnosis was small bowel obstruction secondary to adhesions following his previous abdominal operations. Since his abdomen was acutely tender there was a risk of peritonitis a serious condition. I immediately admitted him to the children’s ward and after rehydration with intra venous fluids and a plain abdominal x-ray had confirmed the diagnosis of obstruction I took him to the operating theatre.
His shunt was functioning normally and the area on the right side of the peritoneal cavity where the CSF was drained was not involved in the adhesions. The adhesions however were iatrogenic, meaning they had been caused by the previous medical intervention. During an operation the boy had undergone a few years earlier, it was routine for the inside of surgical gloves to be dusted with finely powdered chalk by the manufacturer to act as a “lubricant” to facilitate the ease of the surgeon donning them.
Some of this chalk rubbed off the gloves and dropped into the wound and caused a chronic inflammation. In turn this resulted in small bowel loops sticking together, preventing them from sliding smoothly over each other as is normal. When loops of small bowel stick together a kink can occur stopping the flow of the liquid contents through the small bowel resulting in a build-up of fluid above the obstruction and so caused this surgical emergency.
When I operated on my young patient, chalk had not been used as a glove lubricant for several years, so obstruction due to this cause was already in decline. A satisfactory, inactive and absorbable alterative lubricant is now used. Thankfully, chalk as the cause of small bowel adhesions is now consigned to history. The child made a good recovery from the division of his adhesions and returned home a few days later.
Within a few months of this first domiciliary visit requests were coming in at the rate of up to ten a week. By driving round the large catchment area of the Royal Albert Edward Infirmary to visit these patients I came to know Wigan and the surrounding towns and countryside like the back of my hand. Referrals declined after a few years, due to a new Regional Health Authority policy discouraging GPs from requesting consultants to attend home consultations.
Most requests had been for me to urgently see ill and usually aged patients to decide whether they would benefit from being admitted to hospital for an operation or to have investigations that might lead to surgery.
As a result of domiciliary visits about fifty percent of these patients were not fit enough to withstand surgery and would best be made comfortable and cared for at home. Admission to hospital would only have been distressing and of no benefit. Quite often in the early eighties the patient’s GP joined me for the consultation. Being together with their GP was comforting for the patient but more so for the relatives, who were usually grateful for the visit and satisfied that as neither surgery nor admission to hospital would be of benefit. Their natural desire to seek help for their relative had been responded to by both their own GP and the consultant and the fear of missing possible active treatment allayed.
Patients who would benefit from urgent surgery were admitted immediately and if necessary had their operation that night. This was customary as the theatres were routinely open during the evening and night. Often my registrar would operate but if the operation was difficult or complex I would attend to either assist or operate as necessary, all of which enhanced the experience of the registrar and prevented a backlog of patients with emergency conditions competing for operating space during the day which could have resulted in listed cases being cancelled.
The unfortunate result of curtailing domiciliary visits was that many of these unfortunate elderly patients, often with multiple chronic conditions such as diabetes, angina, obesity and respiratory problems were now admitted and caused bed blocking through no fault of their own. Once in hospital they could not be safely discharged, due to any number of medical or social reasons. Not a pleasant situation to be in for a patient.
As domiciliary visits ceased the division of general surgery opened an acute admission ward to which GPs could admit patients direct. This worked well with younger patients who could be discharged later the same day, if they did not need surgery urgently. They were then listed with a date for repair of the hernia if it was prolapsing and at risk of strangulation. Some of the elderly could be discharged if relatives were able to look after them. Frequently this was not possible resulting in long delays while suitably alternative accommodation was found. Following the inception of the NHS most district general hospitals had convalescent homes where patients were sent to recover from surgery or stay while permanent accommodation was found for them. Virtually all these places were unwisely sold in the early eighties putting more pressure on the hospital beds.
Hospitals have a finite number of beds, though in emergencies a few extra can possibly be created. After an operation the length of stay of a patient in the hospital depends on their general condition and what procedure is undertaken. For example, in the seventies a patient following repair of an inguinal hernia would stay in hospital for three to four days. For the last days of his stay the patient would be well enough to help with some of the quasi nursing duties such as taking the tea trolley round to other patients. By the mid-eighties the hospital stay was overnight and by the mid-nineties most hernia operations were day cases with the operation carried out under local anaesthetic.
Another common operation is cholecystectomy, removal of the gall bladder for pain and or inflammation caused by gallstones. This involved a stay in hospital of five days in the eighties, due to a fairly long incision in their upper abdomen. By the late-nineties, young fit patients following use of the laparoscopic technique, which requires very small incisions needing few stitches to close were treated as day patients only.
This illustrates the interesting finding that the smaller the incision the less post-operative pain the patient suffers however extensive the internal operation. This has stimulated the development of very major operations using the laparoscopic or keyhole approach resulting a quicker recovery and a shorter stay in hospital. These good advances led to the hospital beds being occupied by patients following complex major surgery such as aortic aneurysm replacement and unfortunate elderly patients awaiting accommodation in a nursing home. The helpful patients following their hernia repair were no longer to be seen. Overall it was a more efficient use of beds but represented a very heavy workload for the nurses.
Laparoscopic surgery ‘exploded’ onto the surgical scene in the early nineties and all the general surgeons at the RAEI went to St Mary’s Teaching Hospital in London to learn the technique (4). It was a revolutionary change, for the first time surgeons were having to operate using a television screen rather than direct vision, resulting in a switch from working in three dimensional to working in the two dimensions afforded by the flat screen. Open surgery is a “craft” where manual tactile skill is essential and as my chief at Warwick Hospital, John Marsh, was fond of saying part of this skill is, “knowing how fast to go and how hard to pull”. Any deviation from this dictum leads to disaster.
Laparoscopic operating in two dimensions requires different skills to develop anew the feel for delicate tissues. Obviously with the rapid advances in the design of new instruments to carry out the old tasks safely, such as cholecystectomy, were soon learned.
Initially, when American surgeons first started to do laparoscopic cholecystectomies in 1989, the incidence of damage to common bile duct (CBD), a very serious complication, increased fivefold, which was unacceptable (5). From then all surgeons were obliged to carry out a number of these operations under supervision before going solo and this was also applied in the UK. The speed that this new technique spread round the world to become the common approach to gallbladder surgery in most countries was amazing at about five years and technology has been accelerating since.
To learn more I travelled to Dublin in 1991 to gain experience of operating on anaesthetised pigs who have similar gallbladder anatomy to humans (6). Then later after having operated successfully under supervision on a number of patients, all further admissions of patients under my care for cholecystectomy were offered a laparoscopic operation. This was explained in detail but consent was also obtained to convert the operation to a standard open procedure if the operation was proving technically difficult and there was any risk of damage to the CBD.
The reason for this is that patients in Wigan often presented late with their gall stones, when inflammation and thickening of the gallbladder had already occurred, causing it to be stuck to the surrounding tissues, making two dimensional operating treacherous as the CBD could either not be easily seen or even identified at all, so significantly increasing the risk of damaging it.
Having started performing laparoscopic cholecystectomies in the early nineties, the figures for nineteen-ninety-five records show my carrying out 72 cholecystectomies that year, of which 57 were accomplished safely laparoscopically and 15 had been converted to an open procedure, all without mishap (7). In two-thousand, 48 cholecystectomies were carried out, of which six were converted, there were no complications. Thus the experience already gained meant that many of the operations formerly made hazardous, due to inflammation, were now operated on without mishap laparoscopically. I would have expected the conversion rate to tend to zero in the future, however my retirement intervened in two-thousand-and-one. I was reassured with my safety record of never having damaged a common bile duct CBD.
Some years earlier, in nineteen-eighty-three, when the laparoscope and therapeutic endoscopy did not exist, one of my registrars did divide a CBD while removing a patient’s gallbladder. This was very displeasing because he had broken the golden rule by not calling me immediately he was finding the operation difficult and had then compounded his error by proceeding to join the ends together and only letting me know when the patient was awake and in the post-operative recovery room.
If nothing was done, then this patient would probably have made an immediate uneventful post-operative recovery and been discharged home at the normal time. However, as the blood supply to the CBD is complex and the largest contribution usually arises from the duodenal end of the CBD. A divided duct results in an inadequate supply of blood to the CBD above the division. This “ischaemia” will cause this section of the CBD to scar and shrink, so over the next few weeks the passage of bile will be reduced to a trickle and then as the scarring blocks the passage of bile completely causing the patient to become jaundiced. The scarring and inflammation round the CBD would then make an operation to rectify this and relieve the jaundice a major and hazardous procedure.
This was what was running through my head when I took the registrar with me to see the patient straightaway. Fortunately, her husband had joined her so I could explain the situation to them both starting with a heartfelt apology for what had happened. I strongly advised taking the lady straight back to the operating theatre while all the tissues are fresh and easy to handle. My patient and her husband both agreed and signed the consent form.
This re-operation was not difficult and a tube in the shape of a T, was inserted into the CBD to extent as far as possible above and below where it had been inadvertently divided. This tube has a long side arm which is brought out onto the skin so bile can now flow without pressure, either into a bag on the skin or into the gut below. This tube remains in place for three months, during this time any scarring and shrinkage that occurs is prevented from blocking the flow of bile by the presence of the tube. The tube can then be drawn out gently in outpatients, as was done with the patient in excellent health despite all the excitement.
In the infirmary I was fortunate in having an excellent secretary who knew everybody and had an encyclopaedic memory for names and everything that was going on in the firm. Mrs Gillian Bennett sorted out the junior staff and always attended my clinics. It was my habit to dictate a letter after seeing each patient and at the end of the clinic all the letters were signed and posted the same day.
For nineteen years my clinics overflowed with patients, often they did have to wait, but not a second of my time was wasted. If a GP rang up during the clinic concerning an urgent referral the response was always to send their patient up immediately. Naturally the clinics ran over time and the Friday afternoon clinic rarely finished before six-thirty or seven pm. No patient was ever sent away unseen. Neither the nurses nor Gillian, nor the patients complained, I suppose there were one or two complaints over the years but most people were very patient. As a genre, Wigan patients were pleasant, straight forward and willing to take advice. I found them most likeable.
Until just before my retirement GPs used to refer patients to a consultant by name. These referrals were presented to me by my secretary and as I read each letter they were allotted an outpatient appointment depending on the urgency of their condition and any tests that I thought urgent were ordered and the patient informed. As an aside, I had a rule for myself that all letters and communications were seen only once and dealt with at that time to keep paperwork to a minimum.
If a patient was suspected by their GP of having a cancer of the bowel, or if the symptoms described in the referral letter suggested this, then that patient would be seen in the next clinic. Another example for seeing a patient in the next clinic would be if he or she was jaundiced or if a woman had a breast lump.
But to return to patients with cancer of the large bowel. My firm took part, as one of twelve surgical firms in as many hospitals, in a collaborative survey in the north-west between May nineteen-eighty-one and July nineteen-eighty-three. Five hundred patients with cancer of the bowel who had undergone surgery were studied (of which my firm contributed fifty cases).
All my patients did well at the operation, but the distressing fact was that nearly half had come to surgery late in the disease process when their cancer had already spread to lymph nodes or beyond (8). In the eighties there was no other treatment than surgery, there was no effective chemotherapy or radiotherapy.
I immediately investigated why the patients presented to their GPs so late and discovered that the patients had just ignored their symptoms. The study did show that from the date of referral from the GP to my firm and their having a definitive operation was less than a month in 96% of cases, showing that there was no delay in patients receiving treatment once they had first approached their GP. A case was then made for screening for this disease (9).
This was underlined by a conversation I overheard when walking along a hospital corridor one day and found myself behind two senior managers who to my surprise were discussing the long term survival of patients following surgery for cancer of the colon in the North-West of England. They were bemoaning the fact that Wigan had one of the worst results for long term survival for colonic cancer and were implying that the surgeons were better elsewhere. I stopped them and said I had overheard what they were saying and did not agree with their conclusion. They were surprised and said that these were the figures they had received from the Regional Health Authority. I explained the late presentation of local patients to their GPs and asked if the figures had been corrected for the stage of each patient’s cancer at operation. Obviously a person presenting with a cancer confined to a small area of the lining of the colon could expect a complete cure, while a patient presenting after long delay when the cancer had spread to the liver was sadly not going to survive long. The stages were worked out long ago by a London pathologist, Dr. C. Duke who classified the stages from A to D. I asked the managers to let me know when the figures were recalculated (10). To their credit they did so and RAEIs figures were the same as the other hospitals, i.e. survival was disease and not surgeon related.
I made a great effort to start screening the Wigan population for cancer of the bowel. Two large local general practices with about twenty-five thousand patients between them were keen on the idea and applied for permission to spend a small amount of money to buy the packs to test patients stools for occult blood. The screening would start with men aged sixty and then over several years gradually roll out the testing to all men and women over fifty.
The GPs did not receive the go-ahead to buy the necessary test kits as one of our universities was carrying out a trial to see if screening by this method would be successful in reducing mortality. This delay was despite several massive trials in the USA and Scandinavia which had shown that by screening and therefore operating earlier in the disease that the number of patients surviving five years and so likely to be completely cured immediately rose between eighteen and thirty percent. It was a number of years after my retirement that I received such a test pack and was more than ten years after we had unsuccessfully tried to start screening in Wigan.
The way clinically urgent cases when referred by their GP were treated expeditiously, has been described, but if a patient with uncomplicated varicose veins was referred for example, then his or her name was added to my outpatient waiting list to be allocated an outpatient appointment in the future which might not be for a year or longer. This may sound tough, but it is a fact that most patients seeking surgery for varicose veins consider them unsightly and therefore surgery is for cosmetic reasons and not urgent. These patients were free to ask their GP for a referral to another surgeon. My firm had enough operating time for about fifty varicose vein operations a year. So there was no point in seeing more that one patient a week in the outpatient clinics with this condition. Hence the waiting list for non-urgent outpatients. If a patient had complications due to their varicose veins, such as ulcers of the legs or thrombosis, they were seen sooner. The reader can see that the allocation of resources in terms of treatment were carefully allocated by the consultant surgeons, those with cancer or urgent conditions were seen first. All this was done on clinical grounds without targets, but more of that later.
Outpatient clinics were not only to see new patients but also for patients to be “followed up” after operations. It was sensible that my registrar and senior house officer should see patients that I or they had operated on a few weeks before, to check that all was well or if problems such as infection had occurred, to be aware of these problems, recognise them and know how to treat them. This also gave them a feel of how long convalescence should last following different procedures.
The common inguinal (groin) hernia is a case in point as technical advances improved treatment. A manual worker in the early eighties would need to convalesce for at least six weeks before returning to heavy work. Following the development of two new operating techniques for this condition in the nineties. The abdominal wall was strengthened by using a mesh and this technique was taught to all the registrars. This was a good repair and reduced the recurrence rate from five percent to less than one percent. This was cost effective on two counts; firstly, patients could return to heavy work as soon as the wound was comfortable reducing postoperative convalescence by a half and secondly, as the recurrence rate declined, the incidence of people needing a second repair also declined reducing the operative burden on the NHS as well as being good for patients. Psychology and determination also play a part in dictating the speed of recovery, even in the eighties a business man needing to return to work with minimal delay would be back at work within a week and with the new technique was often at work the next day.
There was a patient with rare multiple tumours of the pancreas (Zollinger-Ellison syndrome). These tumours were secreting uncontrollable quantities of the hormone gastrin which then stimulates excessive s causing intractable ulceration of the stomach and duodenum. The only cure was total excision of the pancreas which I carried out. Previously I had removed a parathyroid adenoma from her neck which was causing high calcium levels in the blood and as a result she had developed kidney stones. Ten years later she came for follow to my clinic and complained of moderately severe headaches. Using an ophthalmoscope and looking at her retinas she had papilloedema in both eyes indicating a raised intra-cranial pressure. I arranged for her to see Dr Moore our consultant neurologist the same day, a few days later the neurosurgeons removed a brain tumour. At the time of my retirement she was still well. It was proper and instructive for the registrars to see these patients with complex conditions so they can note what can be done and how the patients had fared.
A pleasure of the week’s work was the Grand Round every Wednesday afternoon. During the morning all the patients for operation on my Thursday and Friday operating lists were admitted and clerked by the students and house officer. The results of tests, such as x-rays, ECGs and bloods were checked. During the ward round we would see all these patients.
I had twin operating theatres on Thursday morning and one of the Thursday lists continued non-stop through the afternoon and as my firm was on take for all emergencies that day the operating sometimes continued through the evening and into the night if needs be. There was also a Friday morning list. I had two other operating lists earlier in the week for more routine operations. Also on the round we would review patients who had undergone major surgery the previous week.
As we reached the end of each patients bed the clerk (student) would present the history which would be supplemented by the house officer or registrar as necessary. The findings on physical examination would be presented and checked. If the patient had physical signs or scars from previous surgery for example, he or she would be examined by the students. There were usually four medical students from Manchester University attached to my firm. If the site or side of an operation was to be marked with an indelible pen; examples being for an inguinal hernia; breast lump for a biopsy or leg for vascular operation, it was marked with the patient wide awake and in agreement. This simple procedure ensured that the correct site or limb was always operated on by my firm.
We would discuss each patient’s signs, symptoms, then diagnosis and the operation. There was also an added dimension to be considered and carefully managed by gastro-intestinal (GI) surgeons, of ileus or temporary paralysis of the gut, after major surgery within the abdominal cavity, for even mobilisation of the gut to gain access to the aorta and great vessels could cause ileus, usually of short duration but may last several days. During this time the patient’s fluid balance must be kept stable and the patient hydrated with the correct intravenous fluids and occasionally if the ileus was prolonged the patient would need to be fed intravenously.
To keep the round lively and to improve the student’s powers of observation there would occasionally be a patient, always a man, with black marks on his arms, shoulders or back. The students would be asked for his occupation at the same time asking the patient not to let on. There was usually silence as they did not know, but one group of students new to the firm all chorused, “He is a miner”. “That’s good” I responded, “the last lot obviously told you,” and everybody laughed. The marks were from injuries where the miners had been hit by falling coal leaving a natural tattoo. In the eighteenth, nineteenth and first seven decades of the twentieth century Wigan had been a major coal producer. Now the last of the mines had been shut but many patients who had been miners still had the scars to prove it.
On other occasions I would ask those who had not already examined a patient to just look at the patient in the bed and give a diagnosis. At the beginning of their attachment the students often said nothing. They were then directed to look at the whites of the eyes, to see they were yellow and since the patient was in a surgical bed then diagnosis must be obstruction of the common bile duct. Further discussion needed tact in front of the patient, as the diagnosis was either obstruction due to gall stones or cancer of the head of the pancreas. In either case I would have told the patient earlier the diagnostic alternatives.
By the end of the eighties endoscopy was available and patients were having their jaundice relieved by a gastroenterologist using an endoscopic technique (ERCP) to gain access to the opening of the CBD into the duodenum and then passing a tube (stent) into the CBD and pushing it through or past the cancer or stones. The bile would now flow again into the gut and over a few days the jaundice would disappear as the stent was left in place. Stones could then often be removed endoscopically, a patient with cancer would also have had biopsies taken to confirm the diagnosis and their suitability for surgery decided.
Before these techniques became available an exploratory operation was the only treatment for obstructive jaundice. If it was caused by stones these would be removed. If cancer a biopsy would be taken to prove the diagnosis and a palliative bypass to allow the bile to flow into a loop of small bowel attached to the CBD above the tumour would enable this. When the jaundice had settled an occasional patient would be suitable for a pancreatectomy.
From the time I was a houseman up to my first post as a registrar not all patients were told their diagnosis if they had cancer and curiously many did not ask. This era of paternalism towards adult patients finally came to an end in the seventies, for it is easier and better to tell patients what is happening to them so they understand the treatment pathway being laid before them or in terminal cases that there is no treatment.
By the end of their three-month attachment the students would have seen a wide spectrum of surgery both great and small on the stomach, colon, rectum, anus, gallbladder, breast, arteries from the aorta to peripheral arteries, varicose veins, thyroid, hernias, children’s operations and some would have seen an operation on the oesophagus, pancreas, parathyroid glands and many more (11). They would have clerked patients and assisted at some operations and with diligent reading they were well placed to pass their examination in surgery.
Thursday, with all day operating, was always an exciting day and it was impossible to predict how it would turn out since the firm was, as mentioned, “on-take” for all emergencies and already had a full elective list of patients for operations in all the theatres. Dr Wyn Jones my consultant anaesthetist would have already seen the patients the previous evening. The first patient would be undergoing anaesthesia from eight-thirty a.m. The surgical team would be ready in theatre before nine scrubbed and ready to gown the patient preparatory to starting the operation at nine. For nine o’clock was the time for “knife to skin”.
The surgical trainees, that is the registrar and senior house officer (SHO) always worked hard and gained much experience. The registrar already had his FRCS and as a rule the SHO had already gained experience with minor and some intermediate operations. The theatres were run in the same way as Professor Bell ran his theatres in Leicester Royal Infirmary while I was a lecturer there. For example, the all-day list might start with a complex operation such as an aorto-femoral bypass graft (12).
The registrar might start this operation by opening the abdomen and proceeding to mobilise the bowel to get access to the aorta lying behind. Meanwhile in the other theatre I would assist the SHO to carry out an intermediate operation, such as a hernia repair and as his experience grew he would carry this out by himself while I assisted the registrar with the vascular case.
In the all-day theatre operating continued without any break until we had finished the list. I would send the registrar and then the SHO for a short rest and bite to eat while I continued to operate. When the opportunity arose for the registrar to operate within his competence I would have a drink and sandwich. However, if the operation was technically difficult I would return immediately. In this way there were no problems and the patients were safe, the NHS was well served and the surgical trainees had a lot of satisfaction with the experience they gained. Part of the skill here was to pick the patients for the two morning lists to match the capability of the registrar and SHO so both theatres could be safely supervised.
As emergencies came into the A & E department during the day, my registrar would go and see those who might be in need of emergency surgery. Perforated duodenal ulcer patients would be rehydrated and added to the end of the elective list. If a ruptured aortic aneurysm presented and he or she was fit enough for surgery, then as time is of the essence, Dr Jones would leave his assistant in charge and take the patient with the leaking aneurysm in hand and prepare him or her to be operated on immediately following the patient currently having their operation. This meant that the list would run way past the official five o’clock finish. Elective cases so displaced by such an emergency were still operated on later and so we continued until all elective and any other extra emergency operations were completed. On average we rarely finished the Thursday list before eight pm and sometimes the list would proceed into the night.
Most patients who rupture an aortic aneurysm do not survive and indeed do not make it into hospital. Half of those who do reach the hospital survived. If the delay of coming into hospital was greater than six hours following the rupture, then the prognosis was worse, but if they had been otherwise fit we would operate.
It was essential to talk to the patient and especially the relatives before undertaking such high risk surgery with an uncertain outcome. There was no cut off age for refusing a patient surgery, if their physical condition prior to operation was satisfactory. It was necessary to explain what the problems were and that without surgery the patient would not survive, but with an operation there was a chance of success although this could not be guaranteed, the very best would be done to bring them through. I taught this to my registrars and told them that if this discussion was neglected and the patient died, then instead of the relatives thinking or saying, “Grandpa went into the RAEI and they did their best, but he died”, they might take the view that something had gone wrong so causing death unnecessarily and say, “He took grandpa to the operating theatre, something went wrong and as a result he died”. They would not surprisingly be aggrieved, because they would not have understood what a dangerous condition the relative was suffering from and that success would be a triumph.
These long days never made me tired or lack concentration, the work was fascinating and never boring. The concept of being tired and making mistakes did not arise. The neurosurgeon Henry Marsh in his famous book, “Do No Harm” wrote that he learned a long time ago that he could, “operate perfectly well in spite of feeling tired”. Going on he says. “People make mistakes when carrying out boring monotonous tasks. Surgery, however trivial the operation is never boring”. With this I wholeheartedly concur. Henry Marsh is not related to my former chief John Marsh.
On most mornings other than Wednesday I was in the RAEI at eight and would carry out a quick business round with the team. Every Saturday morning, I did a full ward-round to see all the patients and to check that all was well with those who had operations in the previous two days. If any were not making the progress expected they would be carefully examined and tests ordered as appropriate. Occasionally a patient would need further surgery which would be arranged later that day and then depending on the urgency or complexity I would carry out or supervise the operation as appropriate.
Some years before while working as John Marsh’s registrar at Warwick Hospital he told me that his only regret was that he had not kept detailed records of the operations that he had carried out over the years. Thinking this a good idea, my secretary, Mrs. Gillian Bennet, gave me an extra copy of every operating lists and this was annotated with details on the day of those operations. After every two hundred operating lists I had them bound into book form for easy reference. Since I had six NHS operating lists a week I collected about three volumes every two years. These documents formed the basis for showing the decline of old general surgery described in the End of the Golden Age of General Surgery (13). So while in retirement and collating the data from my old operating lists, the pattern of work changes over time became clear, demonstrating the changes that the drive towards super-specialisation caused.
There was then a period of five years, between approximately 1992 and 1997 when there were five general surgeons at Wigan on the emergency rota, all capable of carrying out a broad range of surgery including major vascular emergencies. This was the result of the lengthy and sound training given by the teaching hospitals, resulting in the surgeons staffing district general hospitals (DGH) being able to provide a comprehensive service to their local populations. As a result, relatively few patients were referred on to the teaching hospitals. This was the zenith of general surgery in the District General Hospital and the service it provided to the local citizens.
In nineteen-ninety-two, Sir Terence English, a famous cardio-thoracic surgeon who carried out Britain’s first heart transplant in 1979 at Papworth Hospital, in Cambridge was President of the Royal College of Surgeons (PRCS) of England and visited the RAEI to tell his colleagues there of plans to develop a cadre of super-specialists who would be the new consultants. These new consultants would be trained in depth in their area of expertise over a relatively short period of time.
He was well received, but it was pointed out that once this route was implemented it would be difficult to train surgeons to look after patients needing emergency surgery especially those with an “acute abdomen”.
Some years later Lord Darzi, (Baron Darzi of Denham), a consultant surgeon, who advised the then government, indicated that the time to train the new specialists would be reduced from 80,000 hours to 6,000 hours (14).
The old specialty of General Surgery, to which I belonged, would ultimately be split, still under the aegis of general surgery but divided into the following specialties: breast; bariatric; upper gastro-intestinal; colo-proctology; endocrine and thyroid; minimally invasive surgery; trauma and emergency; and vascular surgery.
The difficulty of training surgeons for emergency abdominal surgery once super-specialisation was implemented has proved to be an accurate forecast. Not surprisingly, as a registrar working with my firm between 1980 and 1999 would have carried out many operations in the list given in the paragraph above under supervision, either direct or indirect. As a result, he or she would have had the experience and confidence to diagnose and open any acute abdomen and operate on a ruptured spleen or perforated bowel.
In 2016 a survey was carried out to see if surgeons training to be specialists in breast surgery (oncoplastic breast service) would be confident in carrying out an emergency laparotomy (15). Half of the trainees were not at all confident of acquiring the opportunities to develop this skill and seventy-five percent considered that after appointment as consultants in their speciality they would not have the opportunity to maintain these skills. It is the system that is the problem not the surgeons.
The warnings given to Sir Terence were ignored. It is interesting to note in the “The Bulletin”, the journal of the Royal College of Surgeons of England, of September 2016 that it states that; “There is also a serious under-representation of senior doctors (with) expertise (in) emergency surgery”.
The decline in the volume of breast operations my firm carried can be traced. In the nineteen-eighties between 6 and 21 mastectomies a year were performed, this declined following the appointment of Richard Harland, an excellent general surgeon with a special interest in breast surgery and after 1995 my firm carried out no more of these operations as a new consultant breast surgeon was appointed. As she was our first super-specialist, who was not trained in general surgery, she was unable to join the general surgical rotation looking after emergencies every day of the year.
In paediatric surgery over the years I had operated on children with ulcerative colitis and bowel duplication as well as splenectomies for trauma. Splenectomy had morphed to a salvage operation with the advent of good ultrasound investigations. There was also a steady trickle of babies with projectile vomiting coming on in the first few weeks of life, who had developed a thickening of the muscle of the pylorus at the exit of the stomach so that food was not getting through to the small bowel. These were known as “pye” babies. After ten years of successfully providing a surgical service of Ramstedts operation for these babies, with only one having a significant complication, when the stitches of the abdominal wound gave way and a further operation was required to close the abdominal wall.
I realised one day that I had not seen a “pye” baby for some months and on enquiry discovered that the paediatric physicians had decided to send them all to the local children’s hospital. Unfortunately, both the anaesthetic and surgical skill required was then lost to the RAEI as I was no longer able to teach my registrars how to operate on these babies also the anaesthetist’s skills in anaesthesia for these neonates was lost. I gather most of the routine children’s surgery for example, hernias and undescended testicles (orchidopexy) etc. are now sent to the children’s hospital, which not surprisingly has difficulty coping with the volume of work.
In the last two years before retirement in two-thousand and one I stopped receiving referrals for vascular surgery although continued with the emergencies including rupture of aortic aneurysms. The new vascular surgeon appointed could not technically cope with the work and left. It was worrying that he had been appointed on the strength of glowing references. Finally, eleven years after my retirement, vascular surgery became a sub-speciality in its own right with a dedicated training programme.
A review of Chapter 10 In ‘The training and practise Of a General Surgeon’ shows that in the last two years, my operating output of previous years was reduced by over sixty percent and the inestimable teaching value lost to the trainees. Half my operating lists were allocated to new surgeons. The reduction in hospital beds meant that patients could no longer be admitted the day before their operation, thus the pleasure and usefulness of the Grand Round was a thing of the past. Just before I retired, finding any junior doctor to come round with me to see the patients was impossible as the trainees were now working in shifts. This was a great loss to them not only from a learning point of view but also of establishing a relationship with my patients who were also very much their patients and me. Also lost was the sense of belonging to a surgical entity. “The Firm” was now a thing of the past, the apprenticeship system was truly discarded.
The apprenticeship benefits both apprentice and chief in a symbiosis. It took on average nine months to teach a keen registrar to carry out safely, minor, intermediate and selected major operations. During this period of time I enjoyed teaching and would have to go in to the hospital frequently at night to supervise, assist or operate. Until 1998 my registrars stayed with me for about three years and so in the second and third years the registrar would provide a tremendous service to the NHS and share the burden of work with me and at the same time progress to some complex major operations. It was a benefit to both.
There was another unexpected aspect of my work when for several years in the nineties I was elected by my colleagues to be chairman of the Consultant and Staff Committee. It was during this time that government decided that pay should be negotiated locally. Never having been trade union orientated, I decided to do my best and lead the local negotiations on behalf of the consultants. Brian Livingstone was Vice Chairman and we developed a classic double act. First we decided in advance, after much thought what changes, to our pay and conditions of employment, would give the doctors of the Wigan and Leigh NHS Trust an acceptable outcome if successfully negotiated by us. A series of meetings were then arranged for this purpose with the Chief Executive.
With this careful planning, we decided on our main objectives and then also other things for which we would ask which were not so important to our objectives. However, all were to be negotiated vigorously, but we would gradually give way on the non-essential items, so giving management the feeling they were doing well, aiming that the negotiations would finish having secured our main objectives. Our demands were then presented in advance to management in writing, naturally not indicating which items were important to us.
The negotiating sessions followed a pattern with Brian leading. He was persistent in pursuing our demands and not giving an inch. I would watch the chief executive carefully and his annoyance level could be gauged by his stance and actions. As his annoyance increased he sat forward in his chair glaring and at the same time banged his biro on a blotter and then turned it over to bang the other end. Meanwhile Brian continued on the same track. After a while I would enter the discussion and give way slightly on one of our decoy and unimportant demands. The chief executive would cheer up a bit and concede a point from his side and so we would go on.
The British Medical Association sent an adviser to watch proceedings and they became more and more interested in our progress and started to advise other negotiating teams how to follow our example. We were nearing the end of our negotiations and looked set to win a pay rise. It also appeared that with a bit more effort, we would secure the right for our consultants to have sabbaticals for the first time in the NHS ever!
Then, as is the way with the NHS, government changed its mind and returned to national collective bargaining. I was disappointed that our negotiations came to this abrupt halt, although it brought my trade unionism to an unlamented end.
Another duty as Chairman of the Staff Committee was to be the chairman of “the three wise men” committee, who need not be men and their wisdom will have to be left to others to decide. This committee had the difficult task on occasion to look into the quality of practice of consultant colleagues.
This role was difficult, personal and very time consuming. In the early days of laparoscopic cholecystectomy, the committee was asked to review the work of a colleague and to comment on the standard of the work. All laparoscopic operations at that time were videoed, a decision taken by the surgeons and not management. Now suddenly I had eighty odd tapes, many ninety minutes long to review. Our conclusion after many hours of watching tapes was that the standard was satisfactory and that patients were not at risk.
As management tightened its grip over the medical profession, some consultants were offered paid management roles. For instance, there was to be a director of surgery who would take over the management issues which had previously been done by each group of surgeons appointing a consultant from among their members as part of their expected duties and of course was not paid.
The new Director of Surgery would be paid and this was further sweetened by the pay being pensionable. He or she would continue with a reduced clinical load. At the next staff meeting I advised my colleagues to refuse the pay if they took this appointment. Every consultant at that time had reached the top of their professional ladder and all consultants were on the same pay scale and were equal to all other consultants. This had resulted in the consultant body having a high level of professional satisfaction not being under the orders of another consultant or management in their clinical practice. It was with this in mind that I advised my colleagues that by taking the money they would be in line management not only de facto but also de jure. They would receive orders from above as they would be in line management, only as middle managers without independence. My plea went unheeded and so it came to pass that those who chose to be clinical directors were paid for this.
Targets were first introduced in the late-nineties when management announced that my outpatient waiting list was too long. To be specific, it was the long list of patients with varicose veins waiting for an outpatient appointment. This was the only category of patients referred for surgery on an outpatient waiting list, as I have described earlier. Even though most patients with varicose veins wish for surgery for cosmetic reasons and they were entitled to ask to see another surgeon via their GP it was deemed by the NHS that no-one should wait longer than eighteen months for any operation from the date of referral by their GP. In general, this sounds reasonable but there are consequences. The NHS has been incapable, since its inception, of having a discussion of conditions that perhaps should not be treated by the public purse through the taxes of the citizens and varicose veins (VV) for cosmetic reasons is one such condition.
I was informed by management that the NHS Trust would hire in a doctor from outside to take a series of evening clinics and review the one hundred plus varicose vein (VVs) patients on my out-patient waiting list. After being seen nearly all these patients were added to my operating waiting list. The prospect of doing one hundred extra operations for VVs in the next year was not possible on the routine lists without displacing more urgent cases. Needless to say this arrangement came with a penalty if not complied with.
Any patient who had waited longer than eighteen months on my operating waiting list would be entitled to have the operation carried out in a private hospital by a surgeon from outside the Health Authority’s catchment area. The cost was several thousand pounds per patient and this money would be subtracted from the money allocated by the Health Authority for general surgery in the following year.
When the general surgeons formally met it was realised that failure to comply would result in a reduction to the surgical budget of several hundred thousand pounds. This meant that we would have to close a ward. This of course was crazy and would reduce further the number of operations that the general surgeons could do so exacerbating the problem. So my firm operated on a list of VVs patients at the weekends over the next few months. I have thought long as to why this unreasonable request was complied with by all the general surgeons.
First there was a duty of care to all one’s patients both in the hospital and on the waiting list. At that time the consultant contract was open ended and this included my consultant contract of nineteen-eighty that just said I had “a continuing clinical responsibility for patients in your charge” (17). There was no work life balance, not that this was a subject that I ever thought about. If patients under my care were having post-operative problems for example, I expected to be told so I could decide what should be done and go and re-operate myself if the procedure was beyond the competence of the registrar on duty. This fell within the remit of continuity of care. This is just how it was.
However, management were now imposing and beginning to interfere in surgical practice. By two-thousand managers were firmly in the saddle. This process was the start of disillusionment among consultants leading to loss of morale. Then it spread to the younger doctors with the abolition of the apprenticeship, difficulty of surgeons in training to receive adequate experience and the implementation of the EU working time directive resulting in shift work. All this causing the bitterness and disillusion displayed in the junior doctor’s strikes of two-thousand-and-sixteen. Things have to move forward as the genie cannot be put back into the bottle. The year two-thousand now can now be recorded as the end of the golden age of general surgery.
It is not possible to write this chapter about daily life as a general surgeon in the last decades of the twentieth century without bringing up the problem of the growing burden of litigation. By the nature of the work and due to the frailty and finality of life, not all outcomes of surgery are successful.
If this is the result of negligence as defined by the Oxford English Dictionary (OED) as, “want of attention to what ought to be done or looked after; (or) lack of proper care in doing something”. Then if one or more of these criteria are satisfied, then litigation against the responsible surgeon is justified.
Then there are the vicissitudes of life which can afflict a patient, varying from a nuisance to a grievous deterioration in health or even death. The OED defines vicissitude as, “change; successive substitution of one thing or condition for another taking place from natural causes”. This can occur to a patient of any surgeon however experienced or famous, causing grief not only to the patient and their relatives, but also angst to the surgeon in whom it is accompanied by introspection and a natural feeling of guilt because it has occurred to one of his or her patients, even though all care has been taken.
The first time I became aware of the fact of litigation was when as surgical registrar on duty at the Middlesex Hospital in London in the mid-seventies, a young American woman was brought in following a road traffic accident. She was walking on a pavement when a car mounted the pavement and rolled her between the side of the car and a wall. This unpleasant injury had fractured her pelvis but more seriously had disrupted her anus (18). A very serious and unusual injury that I had successfully repaired layer by layer. When told, a few days later, that she could leave hospital she demurred and wished to stay a further week as this would increase her compensation from the driver of the car. So much so she said that she would probably never need to work again. She went home the same day.
When working for Professor Bell at Leicester Royal Infirmary I had occasionally attended the Coroner’s Court to answer questions about the death of a patient. In this instance the Coroner was searching after the facts and there was never any question of litigation.
I also attended the Coroner’s Court in Wigan on several occasions for similar reasons. Then on one occasion as I came into the court to take my seat, I saw the patient’s relatives accompanied by fully gowned lawyers led by a Queen’s Counsel (QC), which was unusual and looked like trouble.
The man whose death the Coroner was investigating had been sent to see me by his GP a few days before as he was complaining of persistent abdominal pain. He had come alone. My examination revealed that he had large aortic aneurysm, which was tender and he had also recently developed back ache. An aneurysm of this size with these symptoms is likely to rupture in the near future and urgent surgery was indicated. I arranged to see him the next day with the result of tests and asked him to bring his wife with him so I could explain the situation to her as well.
He attended the next day, the tests having confirmed the diagnosis. He was however without his wife. I said it was essential that I should see her so she and his family could be put in the picture. He said he did not want to worry her. I remonstrated that his wife should know, but he insisted that she was not told. The outcome of the consultation was written into his hospital notes and also in my letter to his GP.
The operation was uneventful and his immediate post-operative recovery unremarkable, he was transferred to the Intensive Care Unit as was routine. I was called in the early hours and went to see him. He had a low blood pressure and was peripherally shut down and his only chance was that he had a post-operative bleed. I took him immediately back to the operating theatre and on reopening the incision I found there was no bleeding, so I now suspected that he was suffering from “generalised arterial thrombosis” in spite of his having been given an anticoagulant as was routine during the operation. I removed as much clot as possible from the arteries in his legs and renal arteries which I knew was a forlorn attempt to salvage this man who had developed this rare and un-salvageable complication. His abdomen was closed and he was returned to the ICU where I now met his wife and family for the first time. This was a difficult interview as she knew nothing except that he had had an operation and now he was going to die. She and the family were devastated. I felt terrible as I was his surgeon and could offer no hope. The patient died the next day.
Back in the Coroners Court I was asked to make a statement of what had happened and then the QC was invited to question me. His thrust was that I had been negligent as the wife of the deceased knew nothing. I felt bad about my patient dying but was able to pass to the Coroner my hand written notes and letter to the GP confirming the insistence of the deceased that his wife be told nothing in spite of the operation carrying a five to six percent mortality. I had honoured his privacy against my better judgement. One of the sons of the deceased man came over and thanked me for doing my best which alas was not good enough.
One morning while operating in the old twin theatres at the RAEI my registrar and SHO were operating in the adjacent theatre to me on a patient with varicose veins in both legs which were to be stripped. The registrar was operating on one leg and the SHO on the other. Both had experience of doing this operation and if things were technically tricky I was only six metres away.
I was just finishing an operation when the registrar came through to tell me that the SHO had divided the femoral vein on the leg he was operating on. The femoral vein is the principal vein carrying blood from the leg back towards the heart and he should have divided the long saphenous vein the main varicose vein in the leg which does need to be divided in this operation. A straight forward operation had turned into a possible nightmare for the patient. Why had the SHO not come through and asked before clamping and cutting? This was a matter of supervision and was therefore my fault.
I immediately went through and anastomosed the cut ends together having first checked that there were no clots in the veins further down the leg. Anticoagulation was continued. All seemed well and as soon as the patient woke up I asked for her husband to be called in and spoke to them both. The situation was explained and I told them how sorry I was and that I was responsible. I warned them that further surgery might be needed. By early evening her affected leg began to swell. In the early eighties we did not have ultrasound and the clinical diagnosis was a massive deep vein thrombosis (DVT) in the leg.
We went back to theatre and reopened the vein. Ominously no blood flowed up out of the leg confirming the massive DVT. A compression technique was used to empty the leg veins of clot which were then was washed out with heparinised saline. The vein was again re-anastomosed and anticoagulation continued. Unfortunately, the leg swelled up again by the next day and as it was viable there was nothing further I could do. I kept the lady and her husband up to date and advised them that they were entitled to seek a legal opinion for negligence.
The patient recovered from her operations but always had a swollen leg that was heavy and significantly reduced her walking distance. They never did lodge a complaint. This was an instance where they should have done so and received justified compensation.
Over the years I did receive a few complaints from patients about their treatment. As soon as I learned about this I asked Mrs Bennett, my secretary, to arrange an appointment for the patient and a member of the family to come and see me. Sometimes when I met them the complainants were nervous and angry, so I asked them to tell me about it and listened very carefully to what was said without interruption until they had finished before apologising for their distress and explaining to them what had happened. These were often not matters of great clinical significance and the fact that they had been heard and listened to with a sincere apology and that they were no longer in the dark as to what had happened was usually enough to settle their minds.
Soon after my retirement I received from the RAEI’s legal department a solicitor’s letter concerning a patient who I knew well, he had been in hospital for six months under my care. The letter accused me of negligence in his treatment which had led to his developing a massive pressure sore over his sacrum and also pressure sores on his heels.
I had great respect for the bravery with which this man had borne his serious and debilitating illness. It was true that he had the bed sores, because I had taken him to the operating theatre on several occasions to clean his massive ulcers by debriding them and by the time I retired they were nearly healed.
I was not responsible for his developing these “bed sores”, as they are called, I knew the history and progress of his illness, but I needed the written evidence to dismiss this claim, so I asked the legal department for a facsimile of all his medical records.
His history was that he had been admitted under my care as an emergency with a tender aortic aneurysm. As has already been discussed in this chapter, the treatment is to replace an aneurysm which is at risk of rupture with a graft as an elective procedure, as soon as possible, so giving the patient an excellent chance of full recovery, if delayed there was then a high risk of rupture with a significantly reduced chance of survival. Operation was planned for two days ahead.
Unfortunately, his chest X-ray showed that there was also a massive aneurysm of the thoracic aorta in the chest, also liable to rupture or dissect. His best chance was to have his thoracic aneurysm replaced first and then deal with the abdominal aneurysm. I rang the duty cardio-thoracic surgeon in Manchester who accepted the patient and operated on him that night.
He survived but suffered a severe recognised complication of the operation to replace his thoracic aneurysm (19). This was to develop paraplegia, paralysis of his lower limbs. He had spent a month in that hospital’s intensive care unit in Manchester and there written in the ITU notes was that he had developed the bed sores. This was despite the use every means to prevent bed sores, including an air mattress, regular turning and massage.
He was then returned to my care for repair of his aortic aneurysm. This was quickly accomplished and he made an uneventful recovery from this operation.
Help and advice for his further treatment and rehabilitation for his paraplegia was sought from the local spinal unit who looked after paraplegics. There were unable to help but sent a nurse to advise. She attended and one of our ward cleaners overheard her telling this brave and unfortunate man that I should be sued for negligence.
Now some time later the history of events as documented was discussed at a conference with a QC, in his chambers in London, and this resulted in it being accepted that there was no case to answer. I was very sorry for my patient being put through all this added anxiety due to the ill-informed nurse.
I then requested the legal department of the RAEI to send me the notes of any other complaints against me and was shocked to receive seven bundles of notes and papers. I read them all and could find no evidence to support any of these claims and after collating the evidence, insisted that the Heath Trust defend them. They did and were successful in every case.
The sad fact is that all these claimants were probably motivated by the hope for money, encouraged by some members of the legal profession in return for a substantial cut from any pay out. There are many such law firm’s websites. Even worse this practice was fed by health care trusts across the country who wasted money by “throwing” between three and twenty thousand pounds to such complainants just to go away.
The cost of litigation to the NHS was huge at about £500 million at the end of the last century and by 2014 was in excess of £1 billion. Most, but by no means all, of this money will be recompense to pay for ongoing services in genuine cases of negligence.
I valued my reputation and believe that the late Lord Denning summed it up succinctly. “For an action for negligence against a doctor is for him like unto a dagger.” The fear of litigation has led to the practice of defensive medicine. An age of innocence has also passed.
On my retirement in April 2001, I was replaced by a vascular surgeon, an upper gastro-intestinal surgeon, a colo-proctologist and my extensive practice in thyroid, and parathyroid diseases was taken over by the ENT surgeons.
The current generation of surgeons is beset with major problems. The total great increase in the population of England in the last twenty years. The significant rise in the geriatric population often needing operations while suffering from inter-current diseases. The impact on surgery of the epidemics of type 11 diabetes mellitus and morbid obesity. The increase of dementia. The problems caused by management. Where are the new hospitals and extra hospital-beds? Where are the new medical schools and nursing colleges? The inexorable rise in litigation and problems personal and financial this causes to the profession? (These topics are examined elsewhere on this website).
I enjoyed my career enormously and now in a new era and century I hope that the modern generation of surgeons get the same satisfaction during their career as I did. However, I am still glad that I worked during the Golden Age of General Surgery, albeit at its end.
References.
1. According to the Dictionary of National Biography it is not certain where Myles Standish (1584?-1656) was born. The register of births at Chorley in Lancashire, where it should have been recorded is defaced for the relevant year and it is speculated that this was deliberately done to deprive Myles of his inheritance. In his will Myles bequeathed to his son certain estates in Lancashire ‘surreptitiously detained from him’. (As a commemoration of the Pilgrim Fathers it appears that the purchase of Standish Hall may not have been such a good buy! (Author).
2. The End of the Golden Age of General Surgery 1870-2000. The Training and Practise of a General Surgeon in the Late Twentieth Century. 2015. Publisher Createspace. ISBN 1499531370. Amazon and Kindle.
3. The End of the Golden Age of General Surgery (E of the G A of G S) Chap 10, p. 134-136
4. Ibid Chap. 9, p. 110-111
5. Ibid P. 110
6. Vivisection is illegal in the UK but not then in the Irish Republic. The pigs operated on were destined for the slaughter house and were treated humanely. They enabled surgeons to learn the new technique without risk to patients. Some may consider this wrong which I respect, but it did ensure greater patient safety. Now twenty-five years later the Royal College of Surgeons of England have developed life like models which are used to teach these operations to surgeons so making the use of animals unnecessary, which is a satisfactory advance.
7. Ibid p. 111
8. Ibid p. 117
9. Ibid p 114
10. Ibid p. 115
11. Ibid p. 130
Vulnerability of emergency surgery to the working conditions of new doctors. C Kamau. The Bulletin. 2016, Vol. 98, Issue 6, p 354.
12. Ibid Consultant Contract p. XI
13. Ibid P.75
14. Ibid p.129
15. Review of breast surgery trainees. The Bulletin, RCS. Volume 98, Issue 4,April 2016.Pages 169-171.
16.
17. Ibid. p.XI
18. Ibid p. 51
19. The risk of paraplegia when operating on a thoracic aortic aneurysm arises when clamping the aorta. In a few patients the great segmental medullary artery is the sole blood supply to the lower spinal cord and if its origin is within the thoracic aorta that has to be clamped during the operation, then the blood supply to the spinal cord is cut off and paraplegia may follow.
Index.
Accident and Emergency Department, see Casualty.
Apprenticeship. 40-43, 88.
Architecture of St Thomas’s Hospital. 1871, 10.
Bell, Sir Peter. Professor of Surgery,
Leicester Royal Infirmary. 57.
Bennett, Mrs Gillian. Med Secretary, RAEI. 97.
Betjeman, John. Poet Laureate (1906-1984).
Summoned by Bells. 5.
Bile duct repair. 72-73.
Black, John. FRCS PPRCS. 11.
Carter, Bolton. FRCS Thoracic Surg. LRI
Casualty. 30, 58.
St James’s Hosp. Balham. 53.
Cholecystectomy laparoscopic. 70-72.
Clarke, Dr Paul D. RN. Surg. Commander. 10.
Coccium (Wigan). 60.
Cockett, Frank. FRCS Con Surg. StT’sH. 32.
Collins, Dr. Richard. 12.
Consultant and Staff Committee. 88.
Coote, Professor Sir Ian. Formerly Minister
of Health, Uganda. 24.
Coroner’s Court. 94-95.
Cost of living. Student. 10.
Cotton Mills. 64.
Cranial surgery. 42-43, 59-60.
Cyriax, Dr James (1904-1985). Con Phy.
Med. StT’sH
Dawson, George. Scout Pembroke
College, Oxford. 6.
Darzi, Lord, FRS, FRCS, Con Surg. 85.
Degrees
B.A. in Animal Physiology. 9.
B.M., B.CH. 15.
M.A., D.M.
Devlin, Brendan. (1932-1998). Con
Surg. FRCS. 21.
Domiciliary visits. 67-70.
Dove, John. FRCS 11.
English. Sir Terrence PPRCS. 85, 86.
Examinations.
Primary FRCS. 34.
FRCS, 1972. 44.
Fatigue, effects of. 37-38. 83-84.
General Surgery training. 43-44.
Gowans, Dr. L.J. Oxford University. 9.
Grand Round. 88.
Headhunted. 53-54.
Hillyard, Dr Andrew. 10.
Hippocratic Oath. 15, 25.
Houses
Middleton Square, London. 10
Iver Heath, 23-24.
Gillingham, Kent. 27-28.
Hospital House, Warwick. 34-36.
Crossfields Road, Warwick
Oast House, Brightling Place, Sussex
Bellamy Street, London. 47-48.
Leicester. 54-55, 63.
Cranleigh Standish, Lancs. 63, 65.
Crofters Green, Euxton, Lancs
Criteria for a mortgage. 28. Information Exchange. 10.
Interviews.
Wexham Pk Hospital. 21-22.
Warwick Hospital. 34.
Middlesex Hosp. London. 46.
Kirby, Rayment. Photographer. 4.
Livingstone, Brian. Con. Orth. Surg. RAEI. 88.
Lockhart-Mummery, Sir Hugh (1918-1998),
KCVO, FRCS. General Surgeon. 15
Lymphocytes, circulation of. 9.
Macmillan, Sir Harold. Former PM.
(1894-1986). 16-18.
Marsh, John. FRCS Con. Gen. Surg. WH. 34.
Maybury, Nigel Keith, MA, DM, FRCS.
1969 HO StT’sH.
1969 HO Wexham Pk. H.
1970 CO StT’sH
1970 Prosector of Anatomy.
1970-73 Surg. Reg. Warwick Hosp.
1973-77 Surg. Reg. and Research Fellow, Middlesex Hospital, London
1977-80. Lecturer Surgery, Leicester Royal Inf.
1980-2001. Con. General & Vasc. Surgeon, RAEI.
Middlesex Hospital, London. 46-55.
Middleton Square, No. 19. 10.
Mole, Dr Michael. 10.
Murray, Cecil. FRCS con surg.MH. 46.
Museum, Black, of Crime. 31.
Nevin. Mr R.W. TD, FRCS, Dean & Con.
Gen. Surg. StT’sH. Med.
Sch. 11, 15.
Surg. To HM The Queen’s
Household. 20.
NHS part time contract. 65.
Pembroke College Oxford. 5.
Boat Club. 6,7.
Chapel Quadrangle. 5.
College Barge. 8.
Pengelly, Andrew W. FRCS. 10
Portering at St.T’sH. 8.
Post WWII surgery in the provinces. 65.
Private practice. 16-17, 32.
Prosector. 32-33.
Reed, Dr Peter. FRCP. 21.
Research. 50.
Rise of DGH’s. 66.
Rotas, surgical.
StT’sH. 12, 15.
Warwick Hospital. 34, 36.
Wexham Park Hospital. 23.
Middlesex Hosp. 48-49.
Royal Albert Edward Infirmary, Wigan.
All day operating. 81-83.
Aortic aneurysm rupture. 83.
Apprenticeship, loss of. 1999. 88.
Biliary surgery, impact of endoscopy. 80-81.
Breast Surgery app of super-specialist. 86.
Business Ward-rounds. 84.
Colo-rectal surgery, late presentation. 74-76.
Comprehensive general surgery service. 1992-1997. 84-85.
Decline (final) Gen Surg. 1999-2001. 87.
Grand Round. 78-80.
Iatrogenic problem. 68.
Inguinal Hernia. 77-78.
Litigation. 93-95.
MedicalStaffCommittee, negotiations. 88-90.
Multiple Endocrine Neoplasia. 78.
Negligence, a case of, 95-97.
Negligence claims. 97-99.
Out patients. 62, 76-77.
Targets. 1990s. 91-93.
Varicose Veins. 76-77.
Out Patient clinics. 74.
Paediatric surgery, decline. 1995. 86-87.
Planning Vascular Surg. 66-67.
Planning oesophageal surgery. 66-67.
Records, keeping personal. 84.
Students exposure to surgery. 81.
Super-specialisation planned. 85.
Royal Infirmary, Leicester. 57-60.
St James’s Hospital, Balham. 51-53.
Casualty officer. 52-53
Ruptured spleen. 51-52.
St Thomas’s Hospital & Med. Sch., London.
Emergency surgery. 1969. 18-19.
Pelvic abscess. 19.
Perineal wounds. 20.
Introductory course. 11.
Late presentation to hospital. 18-19.
Living -in as student. 12.
Living in as house officer. 15.
Main corridor. 13.
Mess, junior doctor’s. 16, 31.
Pelvic abscess. 19-20.
Private Practice. 16-18.
Prosector. 21 32.
Sansom, Julian. FRCS. Con. Surg. 38-39
Slack, Sir William. FRCS con Surg. MH. 46.
Spina-bifida. 41-42.
Splenectomy, a case of. 51-52.
Standish, Captain Myles. 63.
Stratford-upon-Avon Hosp. 39.
Stress while operating. 41.
Surgical Firm. 86.
Thomas, Rod. Consultant. 11.
Warwick Hospital 1971-1973.
Duty rota. 23. 36-37.
Hospital House. 34-36.
Operating. 36-37.
Open house
Wexham Park Hospital. 22
Accommodation. 23-24.
Doctor’s mess. 23.
Rota. 23.
Wheeler, Dr Patrick. FRCP. 15.
Wigan
Wigan and Leigh NHS Trust
Wimbush, Doctor FRCP. Med. Superintendent Hammersmith Hosp. 49-50.
Work Scheduled between Xmas eve
and New Year. 65.
Glossary of Abbreviations.
DGH District General Hospital
FRCS. Fellow of the Royal College of Surgeons
LRI Leicester Royal Infirmary.
PPRCS. Past President of RCS.
RCS Royal College of Surgeons of England
Surg. Reg. Surgical Registrar.
RN Royal Navy
StT’sH St. Thomas’s Hospital, London
WH Warwick Hospital
HO House Officer
Con. Gen. Surg. Consultant General Surgeon
RAEI. Royal Albert Edward Infirmary, Wigan
Vasc. Vascular
